INTRODUCTION
The global prevalence of diabetes is increasing; the International Diabetes Federation has reported that 537 million people of total population in 2021, and 643 million people are predicted to become diabetic by 2030[1]. Diabetes mellitus severely damages the heart, blood vessels, eyes, kidneys, and nerves, and causes loss of balance [2], an increased risk of falls [3], reduced quality of life [4], and mortality; hence, the importance of diabetes prevention and management is constantly being emphasized in our society [5].
Patients must continuously perform self-care, which in-cludes understanding diabetes, performing blood sugar tests, following a strict diet, and performing exercises, in addition to medications, to effectively manage the disease [6]. Approaches to encourage patients with diabetes to implement effective self-care regimens include telephone counseling programs [7], individual diabetes education [8], resistance exercise programs [9], mobile applications [10], and diabetes camps [11]. However, it is often difficult to engage participants continuously and maintain their interest throughout intervention programs. To maintain participants’ interest, virtual reality programs with more en-gaging features have been introduced [12]. A study using virtual reality [13] has been conducted recently.
Virtual reality technology uses a computer-generated environment to immerse people/users in a perception of reality [14]. There are two types of virtual reality currently in use: immersive virtual reality, which uses a head-mount-ed display for an immersive experience and non-immersive virtual reality, which uses a 3D graphics environment as seen on console game systems and motion capture cameras [15]. Virtual reality programs have high educational influence and create an immersive experience and increase the concentration of users with their strong simu-lation; hence, they effectively motivate the desire to win and help sustain interest [16]. In addition, they enable continuous education and training [17], providing a safe experience [18]. Therefore, using virtual reality programs that provide patients with diabetes an opportunity to educate themselves and perform effective self-care can help control their blood sugar levels and improve exercise function.
Virtual reality programs are provided through various methods such as Kinect [19], Nintendo Wii [20], immersive virtual reality environment [21,22], wearable sensor and real time visual feedback [23]. These programs have shown a significant decrease in hemoglobin A1c (HbA1c) levels [19,20], and a significant increase in body function [23] and physical activity [21,22] for individuals with diabetes. Therefore, virtual reality is a suitable treatment method for controlling blood sugar levels and improving physical function in individuals with diabetes. Based on these studies, several systematic literature reviews and meta-analyses on the effects of virtual reality programs and games for patients with diabetes were conducted, and the findings corroborated that games and virtual reality programs were effective in motivating healthy behaviors [24], resulting in positive effects on the quality of life, body balance, and muscle strength; however, they had no effect on diabetes-related knowledge or HbA1c levels [25]. But both the aforementioned systematic literature reviews and meta-analyses [24,25] were based on literature up to 2014, with study designs including randomized controlled trials (RCTs) and non-randomized experimental trials, and preliminary studies [24]. Interventions included virtual reality programs and games [24,25]. However, virtual reality is different from mobile or online games in terms of the virtual world, immersive experience, feedback, and interaction [26]; therefore, conducting a systematic literature review and meta-analysis of studies that used virtual reality programs only as interventions, is necessary. This study aims to provide fundamental data for scientific research through systematic review and meta-analysis of the effects of virtual reality programs on patients with diabetes. The study participants were limited to patients with diabetes, and immersive and non-immersive virtual reality programs were applied as interventions, while the control group was the absence of a virtual reality program. The outcome variables were chosen to include various factors, including changes in blood glucose levels, so all possible outcome variables were considered in the paper. randomized controlled trials studies published up to May 2021 were searched.
The purpose of this study is to systematically review the general characteristics (author, country, intervention group, participants, sample size, and so on) of previous studies that have evaluated the effects of virtual reality programs for patients with diabetes and to analyze the effects (HbA1c levels, static balance, dynamic balance, falls efficacy) of virtual reality programs by presenting the effect size of the intervention through a meta-analysis.
METHODS
1. Study Design
This study is a systematic literature review and meta- analysis of RCTs that synthesized qualitative and quantitative data to confirm the effects of virtual reality programs utilized for patients with diabetes. The research plan for this study was registered in PROSPERO (https://www.crd.york.ac.uk/PROSPERO/) and the registration number (CRD42021236581) was obtained on March 12, 2021. Initially, the outcome variable was only HbA1c; however, upon reviewing the literature and discovering that virtual reality had a significant effect on physical function [A1,A2,A5-A7], the study was modified and re-approved by PROSPERO on July 5, 2022.
2. Literature Selection Criteria
Specific questions for the systematic literature review, pertaining to PICOS (Participants, intervention, compar-ison, outcome, and study design) are as follows. Participants of these studies included patients with prediabetes, type 1 or type 2 diabetes, or gestational diabetes. The experimental intervention was a virtual reality program applied to patients with diabetes; hence, all studies using immersive virtual reality with a head-mounted display or non-immersive virtual reality with Nintendo Wii, EyeToy, Xbox, Kinect, and PlayStation were included. Comparative interventions were those that provide only routine care such as exercise and education, and periodic hospital visits that did not involve virtual reality programs. HbA1c level, static and dynamic balance, and falls efficacy were examined to validate the effect of the virtual reality programs. Study design was RCTs. The exclusion criteria were as follows: (1) studies on animals or preclinical trials; (2) studies including patients without diabetes; (3) studies whose original text could be verified; (4) studies not published in Korean, English, or Chinese; (5) non-experiment-al studies such as reviews or observations; and (6) un-published theses.
3. Literature Search
For literature search and analysis, studies up to May 2021 were investigated. English databases such as Pub-Med, EMBASE, CINAHL, Cochrane Central Register of Controlled Trials (CENTRAL), and MEDLINE, Chinese databases such as China National Knowledge Infrastructure (CNKI), Wanfang, and VIP Information, and Korean databases such as DBpia, Korean Studies Information Ser-vice System (KISS), Research Information Sharing System (RISS), and Science on were used to search for published articles or theses. In order to increase the sensitivity of literature search, gray literature such as dissertations, news, and presentation materials were manually searched. In Korean databases, search terms including ‘diabetes (당뇨),’ ‘gestational diabetes (임신성 당뇨),’ ‘prediabetes (전단계 당뇨),’ ‘type 1 diabetes (1형 당뇨),’ ‘type 2 diabetes (2형 당뇨),’ ‘virtual reality (가상현실),’ ‘Wii,’ ‘EyeToy,’ ‘Xbox,’ ‘Kinect,’ ‘PlayStation,’ and ‘Nintendo’ were used (Appendix 1-A). For an efficient search in English databases, MeSH terminology, Boolean operator, and truncation were used. MeSH and text words used in the combi-nation of P (patient) AND I (intervention) AND O (outcome) were as follows: search terms for P (patient) included ‘DM,’ ‘Diabetic,’ ‘Diabetes,’ ‘GDM,’ ‘Type 1 DM,’ ‘Type 2 DM,’ ‘Prediabetic,’ ‘Diabetes, Gestational [MeSH],’ ‘Diabetes Mellitus [MeSH],’ ‘Diabetes Mellitus, Type 1[MeSH],’ ‘Diabetes Mellitus, Type 2[MeSH],’ and ‘Prediabetic State [MeSH]’; search terms for I (intervention) included control or text words such as ‘Virtual Reality [MeSH],’ ‘Wii,’ ‘EyeToy,’ ‘Xbox,’ ‘Kinect,’ ‘PlayStation,’ and ‘Nintendo.’ No specific restrictions were set for search terms for O (outcome) (Appendix 1-B). In Chinese databases, search terms such as ‘Diabetes (糖尿病),’ ‘Diabetes* (糖尿*),’ ‘Virtual Reality (虚拟现实),’ ‘Virtual Reality (假想现实),’ ‘Remote Reality (远程现实),’ ‘Human- Computer Interaction (人机互动),’ ‘Videogame (视频游戏),’ ‘Somatosensory Game (体感游戏),’ ‘Wii,’ ‘EyeToy,’ ‘Xbox,’ ‘Kinect,’ ‘PlayStation,’ and ‘Nintendo’ were used (Appendix 1-C). For the selected literature, the search results were deduplicated. The titles and abstracts were in-dependently reviewed by three researchers: a professor of nursing, a doctor of nursing, and a doctor of Chinese medicine, according to the PICOS and exclusion criteria, for primary selection of studies. Then, secondary selection involved reviewing the full texts of the remaining studies to identify studies to be included based on the inclusion and exclusion criteria. The Chinese literature search and trans-lation were assisted by a Chinese doctoral student in oriental medicine. Any disagreement between the authors pertaining to the selection process was resolved through sufficient discussion, and the opinion of a third author, from the field of oriental medicine, was considered.
4. Qualitative Assessment of Literature
To evaluate the quality of literature used in this study, Risk of Bias the Cochrane risk-of-bias tool (RoB) was used [27], and the analysis was conducted using the Cochrane RevMan Web.
5. Data Analysis
After analyzing the characteristics of studies included in the systematic literature review, data such as First Author, Country, Participants, Age, Sample size, Intervention group, Control group, Main outcome measures, Results, and Author's conclusion were extracted. In a meta-analysis, the random effects model was used, since there was a substantial difference between the selected studies [28]. The effect size was analyzed by a standard-ized mean difference (SMD), mean difference (MD) and Cohen's d. The effect of the outcome variable in this study and the 95% confidence interval (CI) were analyzed using inverse-variance. The effect size was classified as small (effect size of 0.2 or less), medium (effect size of 0.5), and large (effect size of 0.8 or more) [29]. In order to confirm heterogeneity, the forest plot was checked, and the heterogeneity between studies was analyzed using Higgins’ I2 statistic. The I2 value of ≤25.0%, 25.0~75.0%, and >75.0% was assessed as ‘low,’ ‘medium,’ and ‘high’ ‘heterogeneity,’ respectively [30].
Results
1. Characteristics of Studies Included in the Systematic Literature Review
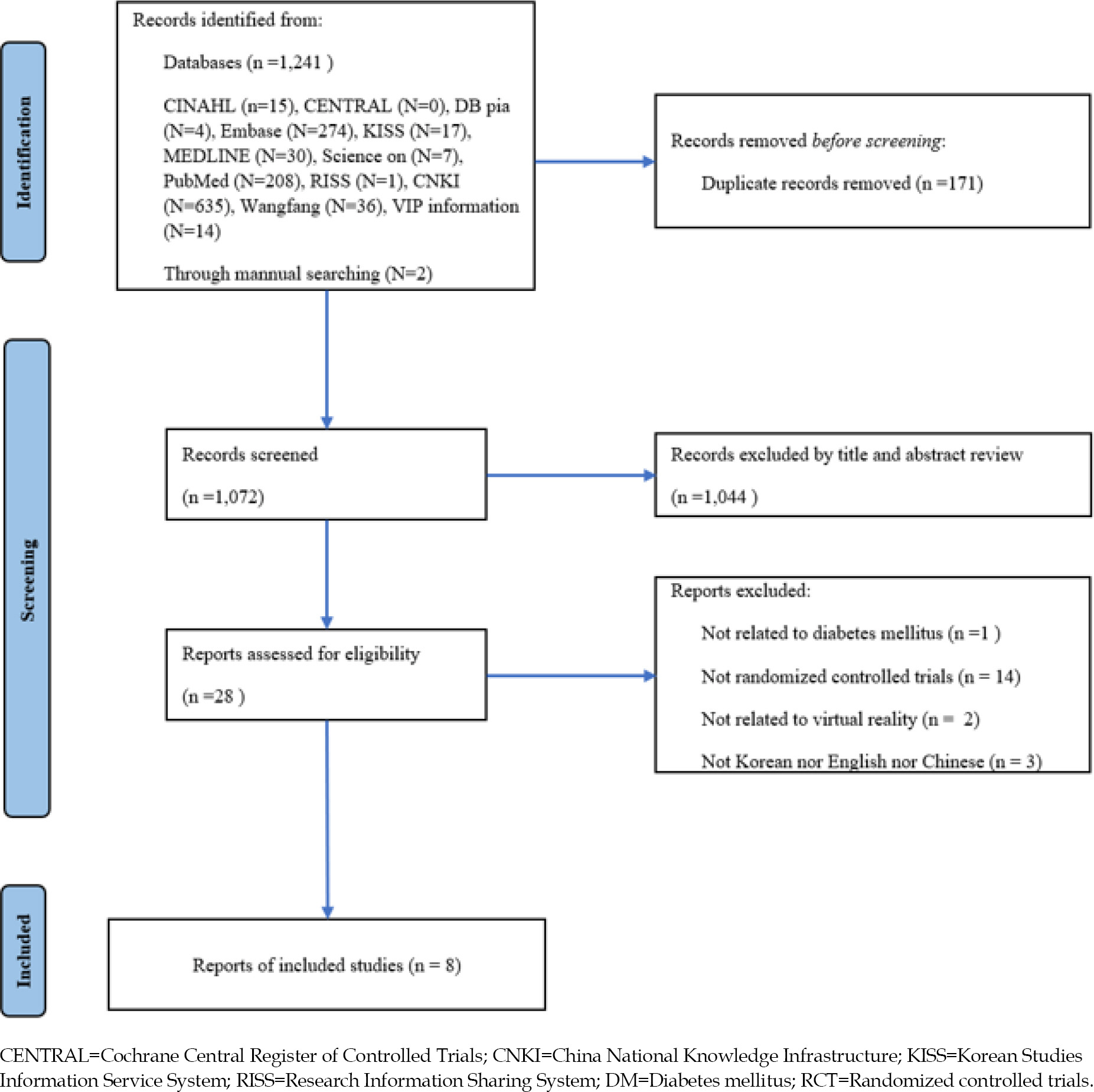
The Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA) were used to describe the status of the step-by-step literature selection process of this study in an easy-to-read and detailed manner [31]. In the database, 1,243 articles were searched. After excluding 171 duplicates, 1044 studies were excluded according to the PICOS and exclusion criteria. After the full texts of articles were reviewed, eight studies were finally selected. Qualitative analysis was performed on the eight selected studies, and the results of six of these studies were included in the meta-analysis (Figure 1).
All eight studies were journal articles and were published in 2010 or later. Three studies were conducted in the United States [A5-A7], four studies were conducted in Asia [A1,A2,A3,A8], two studies in South Korea [A1,A2], two studies in China [A3,A8], and one study was conducted in Germany [A4]. In terms of the study Participants, there were seven studies on type 2 diabetes [A1-A6, A8] and one study on prediabetes [A7]. Two of the studies on type 2 diabetes involved participants who were patients with a complication of diabetic neuropathy [A5]. In terms of age, six studies included participants aged ≥60 years [A1,A2,A4-A6,A8], and two studies included participants aged 34-55 years [A3,A7]. Regarding the type of virtual reality used, none of the studies used immersive virtual reality programs using head-mounted displays. All eight studies were non-immersive virtual reality program studies using 3D stereoscopic images, gaming consoles, motion capture cameras, and body-tracking sensors. Regarding the methods for executing the virtual reality programs, two studies used PlayStation and EyeToy [A1,A2], three studies used Nintendo Wii [A4,A6,A7], one study used sensor-based interactive exercise training [A5], and two studies used Kinect [A3,A8]. In terms of years and countries where certain virtual reality programs were used, PlayStation and EyeToy were used in South Korea in 2012 [A1] and 2013 [A2]. Nintendo Wii was used in Germany in 2013 [A4] and in the US in 2018 [A6] and 2019 [A7]. Sensor-based interactive exercise training was used in the US in 2015 [A5], and Kinetic was used in China in 2015 [A3] and 2020 [A8]. The application time for the virtual reality program was 30 min in two studies [A3,A4]; 35 min, five times a week in one study [A8]; 40 min, three times a week in one study [A6]; 45 min, twice a week in one study [A5]; and 50 min, twice a week in two studies [A1,A2]; and 50 min, three times a week in one study [A7]. The duration of the virtual reality intervention was 15 days in one study [A3]; four weeks in one study [A5]; six weeks in one study [A8]; 10 weeks in two studies [A1,A2]; and 12 weeks in three studies [A4,A6,A7]. The minimum number of samples in each experimental and control group ranged from 14~93, and the total number of samples ranged from 30~176. The control group received routine treatment in two studies [A4,A5]; diabetes education in two studies [A1,A2]; routine treatment and diabetes education in one study [A3]; routine treatment in one group and general exercise in one group, with two control groups in one study [A7]; general exercise in one study [A6]; and rehabilitation treatment and balance training in one study [A8]. The main outcome variables of this review were HbA1c, static body balance, dynamic body balance, and falls efficacy. Among the eight studies included in the qualitative analysis, three studies measured HbA1c levels as an outcome variable [A3,A4,A7], five studies measured static body balance [A1,A2,A5,A6,A8], two studies measured dynamic body balance [A2,A8], and two studies measured falls efficacy [A2,A5]. Regarding the effect of the application of virtual reality programs for patients with diabetes, HbA1c level was used to measure blood glucose control. Among body balance scales, static balance scales included the Postural Sway and One-Leg Standing tests, and dynamic balance scales included the Berg Balance Scale. The falls efficacy scales included the Falls Efficacy Scale-International (FES-I) and the Modified Falls Efficacy Scale (MFES) (Table 1).
Table 1.
Summary of the Virtual Reality Programs' Effects on HbA1c Levels, Balance, and Falls Efficacy in Patients with Diabetes
| No | First author (year)/ Country | Participants Age (year)/ Mean or range | Intervention group Intervention Method | Control group | Main outcome measures | Results | Author's conclusion |
|---|---|---|---|---|---|---|---|
| A1 | Lee (2012)† South Korea | Type 2 DM (A) 73.8(B) 74.3 | (A) PlayStation, EyeToy (50 min twice a week for 10 weeks) + Health education (N=27) | (B) Health education (N=28) | Static balance (postural sway) | MD -20.2895% CI:[-25.51, -15.05] | ‘The virtual reality-based program… an effective intervention for improving the balance of the elderly with diabetes…’ |
| A2 | Lee (2013)† South Korea | Type 2 DM (A) 73.78(B) 74.29 | (A) PlayStation, EyeToy (50 min twice a week for 10 weeks) + Health education (N=27) | (B) Health education (N=28) | Dynamic balance (BBS) | MD 2.2795% CI:[1.00, 3.54] | ‘The virtual reality exercise program can be used to reduce the risk of falls in elderly individuals with diabetes’ |
| Falls efficacy (MFES) | MD 1.0895% CI:[0.45, 1.71] | ||||||
| Static balance (one-leg standing) | MD 5.8095% CI:[1.99, 9.61] | ||||||
| A3 | Deng (2015)† China | Type 2 DM (A) 35~55(B) 34~54 | (A) Kinetic (30 min/day for 15 days) + Usual care + Health education (N=30) | (B) Usual care + Health education (N=30) | HbA1c | MD -0.9095% CI:[-1.09, -0.71] | ‘Strengthening diabetes exercises combined with somatosensory tracking device Kinect… is beneficial to reduce HbA1c…’ |
| A4 | Kempf (2013)† Germany | Type 2 DM (A) 61(B) 60 | (A) Wii Fit Plus (at least 30 min/day for 12 weeks) + Routine care (N=93) | (B) Routine care (N=83) | HbA1c | MD 0.1095% CI:[-0.14, 0.34] | ‘Wii fit plus was able to motivate T2DM patients to improve glucometabolic control…’ |
| A5 | Grewal (2015)† USA | Type 2 DM + DPN (A) 62.58(B) 64.9 | (A) Sensor-based interactive balance training (45 min training session, twice a week for 4 weeks) + Standard of care (N=18) | (B) Standard of care (N=16) | Static balance (postural sway) | MD -0.4895% CI: [-1.45, 0.49] | ‘… exercise training through an interactive virtual interface with real-time visual feedback… significantly improve postural balance in people with diabetic peripheral neuropathy… may reduce the risk of fall.’ |
| Falls efficacy (FES-I) | MD -4.5395% CI:[-11.86, 2.80] | ||||||
| A6 | Morrison (2018) USA | Type 2 DM (A) 66.1(B) 67.8 | (A) Wii Fit Balance Board (40 min, thrice a week for 12 weeks) (N=14) | (B) Supervised training (N=32) | Static balance (postural sway) | (A) Positive change significantly (p<.05)(B) Positive change significantly (p<.05) | ‘Both 12 weeks of supervised balance training and unsupervised, at home balance activity (using the Nintendo Wii Fit)… reduces falls risk in older T2DM individuals.’ |
| A7 | Bock (2019) USA | Prediabetics (A) 49.3(B) 52.3(C) 52.0 | (A) Wii Fit plus (50 min, thrice a week for 12 weeks) (N=27) | (B) Treadmill, cycling (50 min, thrice a week for 12 weeks) (N=28) | HbA1c | (A, B) p<.05(B, C) NS (A, C) p<.05 | ‘Exercise videogames… improve management of blood glucose…’ |
| (C) Mailing on general health topic (N=29) | |||||||
| A8 | Zeng (2020)† China | Type 2 DM + DPN (A) 63.40(B) 64.67 | (A) Doctor Kinetic (35 min/day, 5 times/week) + Routine care + Integrative rehabilitation + Conventional rehabilitation (35 min/day, 5 times/week) for 6 weeks (N=15) | (B) Routine care + Integrative rehabilitation + Conventional rehabilitation (35 min/day, 5 times/week) for 6 weeks (N=15) | Dynamic balance (BBS) | MD 2.8095% CI: [0.48,5.12] | ‘Virtual sports games can effectively improve the static and dynamic balance function of elderly DPN patients…’ |
| Static balance (postural sway) | MD -0.2495% CI:[-0.40, -0.08] |
2. Qualitative Assessment of Literature
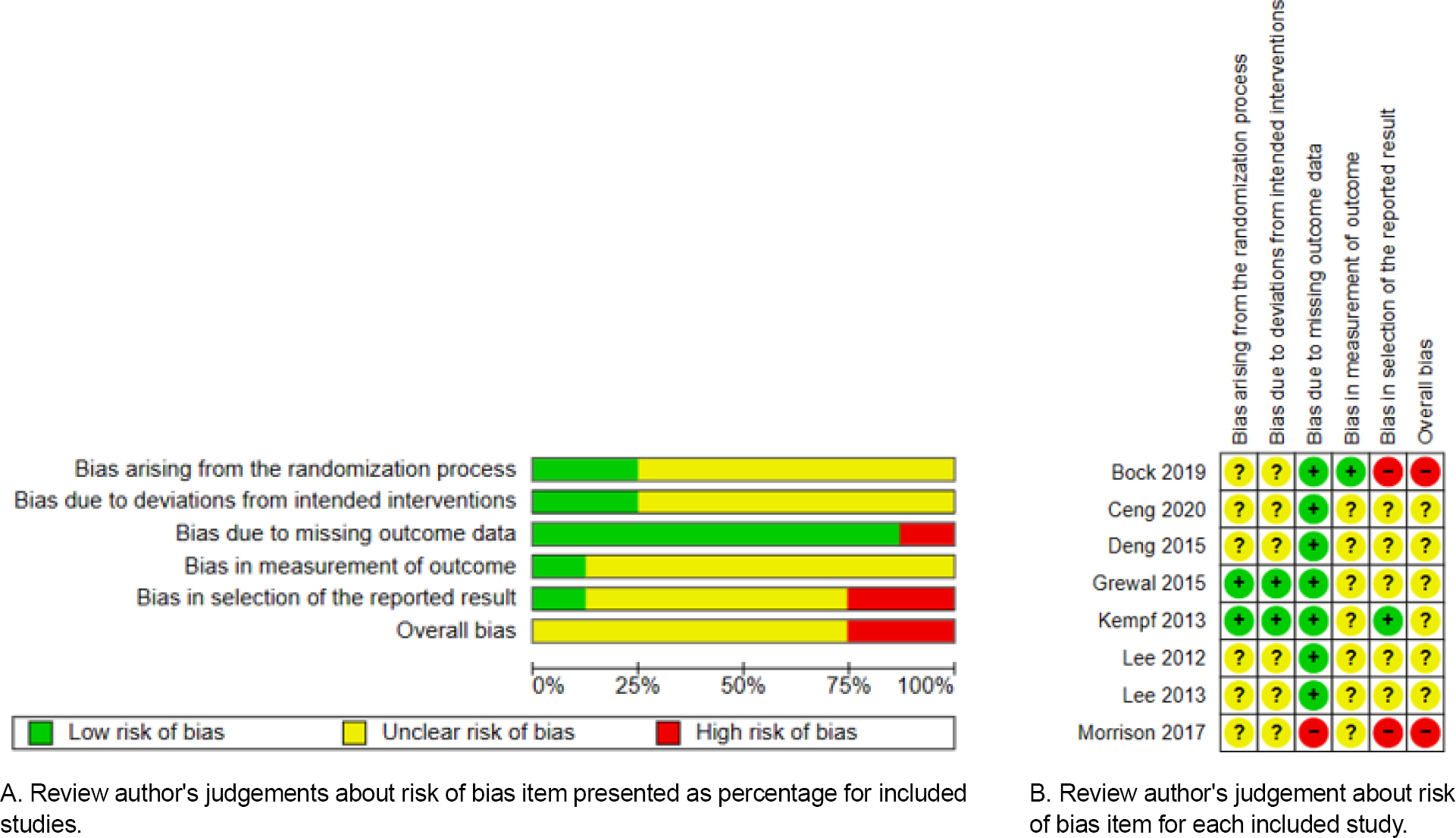
The results after entering the eight selected studies into the RevMan software, according to the quality evaluation criteria are as follows (Figure 2). In terms of bias arising from the randomization process, the RoB was evaluated as ‘low’ in two studies; the allocation sequence was random and concealed until participants were enrolled and as-signed to interventions. Six studies were evaluated as ‘un-clear,’ since there was no mention of allocation conceal-ment. In terms of bias due to deviations from intended interventions, the RoB was evaluated as ‘low,’ in two studies while the remaining six studies did not mention blinding of caregivers and people delivering the intervention, and the RoB was evaluated as ‘unclear.’ As a result of analyzing bias due to missing data, one study had a ‘high’ RoB since the dropout rate of 54.0% in experimental group. In the bias in measurement of the outcome, seven studies were evaluated as ‘unclear,’ since there was no mention of blinding of the outcome evaluation. In terms of bias in selection of the reported result, two studies had a ‘high’ RoB since the results were incomplete and could not be used for meta-analysis. In the remaining six studies, the RoB was assessed as ‘unclear’ since the trial registration number was not included.
3. Effect Size of Virtual Reality Program Applied for Patients with Diabetes on HbA1c Levels
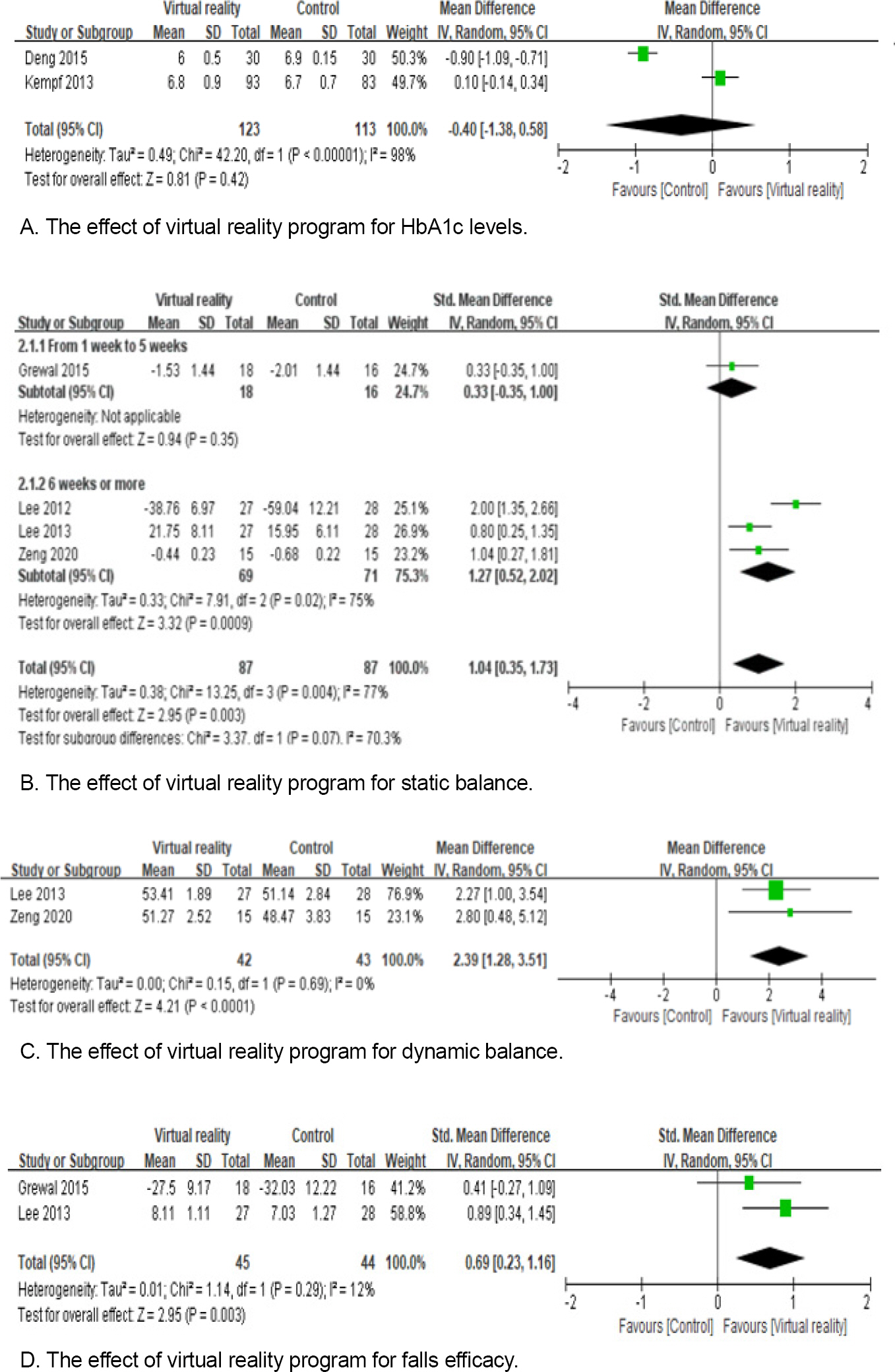
The effect size of the experimental group with the virtual reality program applied and the control group without the virtual reality program applied was -0.40 (n=236, 95% CI: -1.38~0.58), which was not statistically significant (Z=0.81, p=.42). The heterogeneity between studies was high with Higgins’ I2=98.0% (Figure 3-A).
4. Effect Size of Virtual Reality Program Applied to Diabetics on Balance Ability
1) Static balance
Postural sway and one-leg standing test were used to measure static balance. Since the two scales oppose each other, they were adjusted using a minus sign. The effect size of the experimental group with the virtual reality program applied and the control group without the virtual reality program applied was 1.04 (n=174, 95% CI: 0.35~1.73), which was statistically significant (Z=2.95, p=.003). However, a subgroup analysis was performed due to the high heterogeneity among studies with Higgins I2=77.0%. This analysis was conducted by dividing the period of application of the virtual reality program into two groups; one to five weeks and more than six weeks. The experimental group that participated in the virtual reality program from one to five weeks demonstrated an increase of 0.33 (n=34, 95% CI: -0.35~1.00) in static balance when compared to the control group, with no statistically significant difference (Z=0.94, p=.35). The experimental group for which the virtual reality program was applied for more than six weeks demonstrated an increase of 1.27 (n=140, 95% CI: 0.52~ 2.02) when compared to the control group, with a statistically significant difference (Z=3.32, p<.001) (Figure 3-B).
2) Dynamic balance
The effect size comparing the experimental group with the virtual reality program applied and the control group without it being applied was 2.39 (n=85, 95% CI: 1.28~ 3.51) and was statistically significant (Z=4.21, p<.001). The heterogeneity between studies was low, with Higgins’ I2=0.0% (Figure 3-C).
5. Effect Size of Virtual Reality Program Applied for Patients with Diabetes on Falls Efficacy
The methods for measuring falls efficacy in this study included the FES-I and the MFES. Since the two scales op-posed each other, they were adjusted using a minus sign. The effect size of the experimental group with the virtual reality program applied and the control group without it being applied was 0.69 (n=89, 95% CI: 0.23~1.16), which was statistically significant (Z=2.95, p=.003). The heterogeneity between studies was low, with Higgins’ I2=12.0% (Figure 3-D).
The asymmetry of the funnel plot could not be con-firmed. According to Higgins, this test required at least ten studies to be included in the analysis [32].
DISCUSSION
This systematic literature review and meta-analysis was conducted to confirm the methodology and effect of the virtual reality program for patients with diabetes. Eight studies were included based on the selection criteria and were qualitatively analyzed, and six studies were included in the meta-analysis.
These eight studies had a low risk of missing outcome data. The randomization process, deviations from intended interventions, measurement of the outcome, and selection of the reported results were not described in the literature; hence, identifying the risk of these biases was difficult. In future RCTs, randomization and blinding should be strictly designed to avoid investigator bias, and this information should be well-elucidated in the literature. Additio-nally, the registration number of the clinical trial and re-lated information should be provided to identify potential bias.
Qualitative analysis of all eight studies used non-immersive virtual reality interventions. Although immersive virtual reality programs have a higher immersive experience, studies that applied them were limited since the de-velopment of such programs were challenging. An immersive virtual reality program was applied only in one non-randomized experimental study, which included exercise, education, and treatment for patients with diabetes [13]. Therefore, conducting a randomized trial, for patients with diabetics in the future is necessary to confirm the effect of this program.
HbA1c were analyzed to confirm the effect of the virtual reality program on the blood sugar control of patients with diabetes. HbA1c level were decreased in the experimental group when compared to the control group, although it was not statistically significant. In a previous systematic literature review [25], reduction in HbA1c levels was not observed when games and virtual reality programs were employed. Earlier studies could not validate the effect of virtual reality programs on HbA1c levels, though two studies included game interventions [33,34]. In the study that employed an immersive virtual reality program for 12 weeks [13], a study that administered a 12-week program using Kinect [19], and a study that administered a 12-week program using Nintendo Wii [20], HbA1c levels were significantly reduced due to the experimental intervention; however, these were non-randomized trials. Therefore, in order to confirm the effect of the virtual reality program on HbA1c levels, strict experimental studies will be needed in the future. In addition, education on medical treatment for diabetes, lifestyle improvement, diet, and exercise therapy are important for diabetes management [35]. Since virtual reality programs, including diabetes education, are Reportedly effective in reducing HbA1c levels [13], it is necessary to develop these modalities.
Static and dynamic balances, and falls efficacy were analyzed to confirm the effect of the virtual reality program on the physical ability of patients with diabetes. In a study that provided a virtual reality exercise program for five weeks, the experimental group demonstrated no significant difference when compared to the control group [A5]. In other studies, significant improvements in static balance indicated that virtual reality exercise programs should be provided for more than six weeks [A1,A2,A8]. Previous studies that employed vibration stimulation resistance exercise [36], resistance exercise using a sling [37], and aqua therapy [38] reported significant improvement of balance after a six-week or longer exercise intervention. Thus, virtual reality exercise programs should be designed as a six-week or longer program to enhance balance.
This study is significant because it confirms the effect of virtual reality programs for patients with diabetics who needed continuous management by systematically reviewing the research that applied these programs. Conversely, an insufficient number of randomized controlled experimental studies applying virtual reality programs, which made presenting sufficient evidence difficult, is a limi-tation of this study.
CONCLUSION
The findings indicated that the effect of virtual reality programs in reducing HbA1c levels could not be con-firmed; however, it was effective in improving balance ability and falls efficacy. Based on these results, we recom-mend the following. Subsequent studies should develop virtual reality programs not only for exercise but also for education about diabetes mellitus to promote effective management of diabetes mellitus. Further, these programs should be designed to be at least six weeks to improve physical functioning of individuals with diabetes mellitus. In the future, strictly randomized and blinded studies are necessary, and a repeat systematic review and meta-analy-sis is recommended after the accumulation of such studies.