Review of Diabetic Foot Complication Assessment Tools Developed from 2007 to 2016
Article information
Abstract
Purpose
The purpose of this study was to analyze the attributes and psychometric properties of newly developed diabetic foot complication assessment tools. The attributes of diabetic foot complication assessment tools were evaluated using a systematic review.
Methods
The search terms: “diabetes mellitus” and “foot ulcer” were retrieved using Boolean operators of “and”, “or”, and “not”. The search was limited to articles published between 2007 and 2016. The literature was analyzed by division of methodological characteristics, instrumental characteristics, and item and stratified outcome characteristics.
Results
Six assessment tools were found for diabetic foot complications. Only three of the six tools presented the evidence in terms of validity and reliability. In all six tools, “ulcer” was the measured item with the highest frequency, but the contents of items varied. The six identified tools focused on assessing current physical symptoms, but not on predicting diabetic foot complications.
Conclusion
Preventive foot self-care should be used to predict diabetic foot complications before symptoms appear. Moreover, the reliability and validity of existing tools should be verified in terms of discrimination, prediction, and evaluation.
INTRODUCTION
In diabetes mellitus (DM), unsuccessful glycemic control over a long period of time can cause diabetic neuropathy, peripheral vascular dysfunction, or occlusion, which can lead to diabetic foot [1]. The incidence of diabetic foot ulcers is approximately 2% per year, and the lifetime incidence for diabetic patients is 15~25% [2]. 50~70% of foot amputations are preceded by diabetic foot ulcers [3]. When the foot is amputated, there is a 60% chance of amputating the contralateral foot within five years, with the 5-year mortality rate around 40% [4-6]. The likelihood of leg amputation for patients with DM is 10.1 times higher than for patients without DM, with a 7.8 times higher chance of developing diabetic foot complications [7]. Furthermore, the annual average total cost of treatment is 2 times higher for patients with DM, and the number of hospital days is 1.6 times higher than it is for patients without DM [7]. DM results in a high prevalence rate of diabetic foot complications, serious aftereffects such as amputation, long-term treatments, financial problems caused by high treatment costs, and social and psychological stress for patients and their families [8].
The prevalence rate and treatment costs of diabetic foot complications can be reduced by regular foot examinations, regular screening for prevention of diabetic foot ulcers, differentiation of high-risk patients, and lesion treatment; and additionally, the incidence of leg amputation can be decreased to 50%[1]. Accurate assessment is essential for precise identification of risk factors for foot ulcers, as well as for discerning high-risk groups and ensuring that ulcers do not lead to amputation [9]. Diabetic foot complications need to be managed in a way that monitors the present condition while also screening for risk factors early to prevent the patient from becoming high-risk for amputation [9]. Therefore, the use of standardized assessment tools for objectively evaluating and discerning diabetic foot complications is an important clinical practice.
Tools that were developed few decades ago for assessing diabetic foot complications include the Pressure Sore Status Tool (PSST) [10], Pressure Ulcer Scale for Healing (PUSH) [11], Wound Healing Scale (WHS) [12], Sussman Wound Healing Tool (SWHT) [13], and Bates-Jensen Wound Assessment Tool (BWAT) [14]. Unfortunately, these tools were designed to assess for wound change, not for early screening of diabetic foot complications such as preventive behavioral factors (i.e., regular skin check). Recently, they are not often used in clinics because the tools are complicated and cumbersome. On the other hand, the Wagner system [15] and the University of Texas Diabetic Wound Classification [16] are used more frequently than tools introduced above because of they are easy to assess and simple. The Wagner system and University of Texas Diabetic Wound Classification can assess the ulcer depth and the presence of osteomyelitis or gangrene by using grading system from 0 to 5 for foot, but it is limited in identifying preventative behavior and early detection of foot changes needed to make a clinical judgment [17,18].
Data that have been consistently well-researched using standardized assessment tools can be used to monitor changes in the patient and may be useful for communication between multi-disciplinary teams [19]. Despite the number of patients with DM that have suffered from diabetic foot complications, risk classification tables that can effectively screen for early cases of diabetic foot have been limited [8].
Due to the necessity of developing an assessment tool that can classify, predict, and evaluate diabetic foot complications, we conducted a literature review with the aim of systematically evaluating the psychometric properties of diabetic foot complication assessment tools. The specific goals of this study were a) to analyze the methodological characteristics and psychometric properties of the included assessment tools, and b) to classify the items of the assessment tools.
METHODS
1. Study Design
The study design was a systematic literature review of the contents and properties of diabetic foot assessment tools.
2. Search Strategy
The two authors independently searched for articles related to diabetic foot complication assessment tools that were published between 2007 and 2016 in the CINAHL Database, PubMed, Embase, and Cochrane Library Database. The clinical practice guidelines for the diabetic foot were revised in 2006 and several tools were developed to reflect the new guidelines, limiting the period of article extraction. The search terms of “diabetes mellitus” and “foot ulcer” were retrieved using the Boolean operators “and”, “or”, and “not”. MeSH terms and synonyms were checked prior to performing the search.
3. Inclusion Criteria and Exclusion Criteria
Inclusion criteria were as follows: 1) the study included a standardized assessment tool for diabetic foot complications that was developed within the past 10 years, and 2) the publication was written in English. Exclusion criteria were as follows: 1) intervention studies and cohort studies were excluded; 2) publications such as dissertations, announcements, and independent volumes were excluded; and 3) tools that placed more importance on assessment for complications other than diabetic foot complications were excluded.
4. Data Extraction and Evaluation
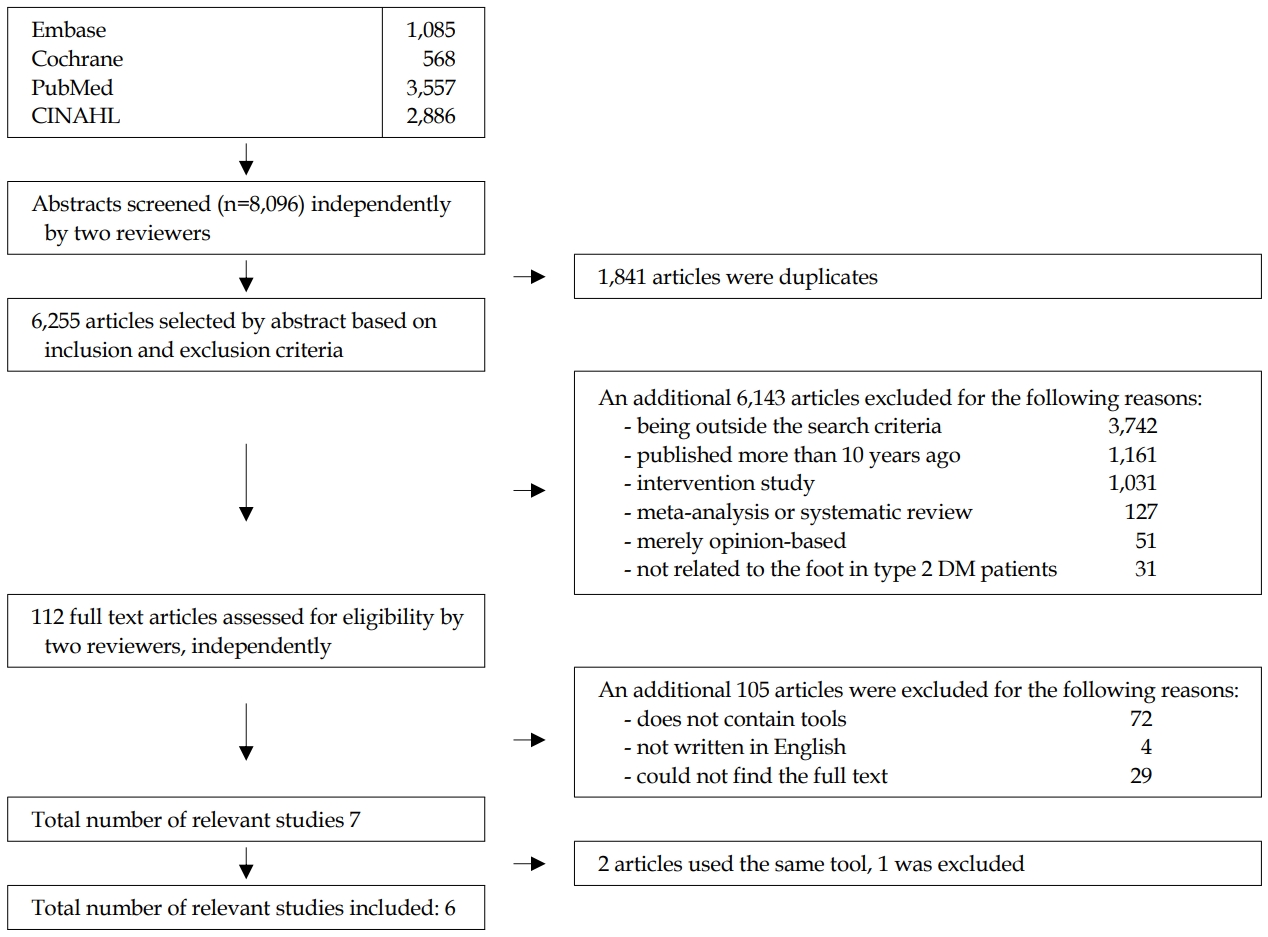
The literature search was performed in two stages. First, the titles and abstracts were reviewed for relevancy to this study. Next, the full article was reviewed; if it matched the inclusion criteria, it was selected. A total of 8,096 results were found from the following: 1,085 results from Embase, 568 results from Cochrane Library CENTRAL, 3,557 results from PubMed and 2,886 results from CINAHL. Endnote X7 identified 1,841 duplicate results, which were excluded. The two researchers then reviewed the abstracts independently and selected relevant papers according to the inclusion criteria (studies that included tools to assess diabetic foot complications). In the process of checking the titles and abstracts, publications that were intervention studies, meta- or literature reviews, published more than 10 years ago, or mainly opinion articles were excluded. Accordingly, 6,143 results were excluded. In the second step, a review of the entire article, the authors excluded an additional 105 articles for reasons that included, among others, being written in a language other than English or not having included the assessment tool. Ultimately, a total of seven papers were selected. However, two of these papers included the same tool; therefore, the one that was published more recently was selected, leaving a final total of six tools. Two independent researchers conducted the literature search process. When there were differences in opinion, these were resolved through discussion between the researchers (Figure 1).
5. Ethical Considerations
This study protocol was approved by Institutional Review Board (IRB No 2-1046881-A-N-01-201703-HR-007-09) of C-University.
RESULTS
1. Methodological Characteristics
A total of six tools were selected as standardized assessment tools used for diabetic foot complications: The Foot Assessment Form, the revised version of Basic Foot Screening Checklist (BFSC), the Saint Elian Wound Score System (SEWSS), the United Kingdom Screening Test (UKST), Screening for the High-Risk Diabetic Foot: A 60-Second Tool, and the New DFU Assessment Scale (DFUAS).
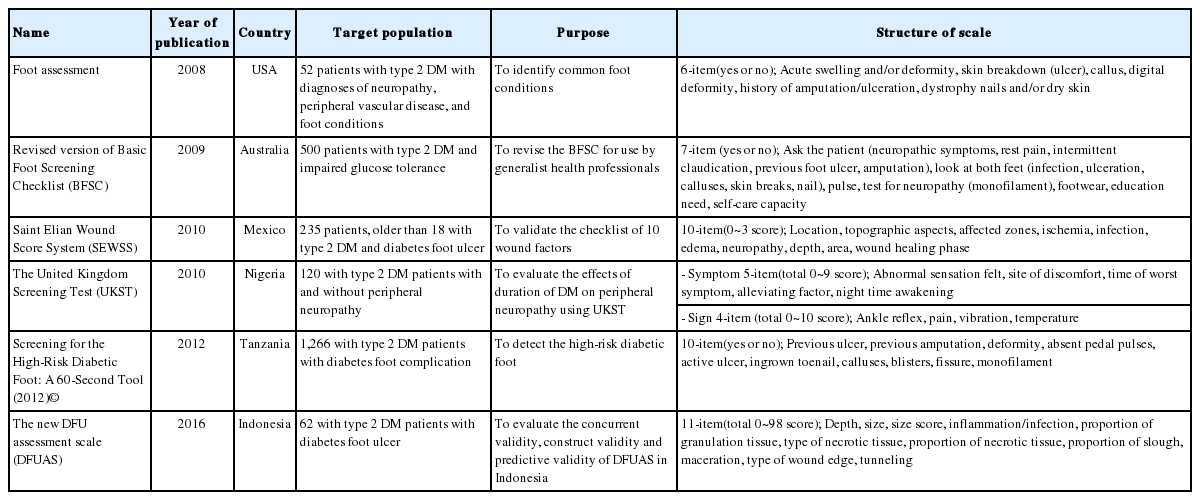
The tools were developed between 2007 and 2016. By country, there was one tool each from the United States, Mexico, Australia, Nigeria, Tanzania, and Indonesia. These tools were all developed for type 2 DM and were used to assess a population ranging from 52 to 1,266 patients. Methodological characteristics, including evaluation purpose and structures of items in each tool, are presented in Table 1.
2. Psychometric Properties
The total number of tool items ranged from 6 to 11. To examine the psychometric properties, the validities and reliabilities were identified. Among the six tools, the Foot Assessment Form and UKST did not evaluate both reliability and validity (Table 2).
The BFSC and DFUAS evaluated validity by calculating the sensitivity (54% and 89%, respectively), specificity (77% and 71%, respectively), and positive predictive value (82% and 86%, respectively). The BFSC and SEWSS calculated reliability by a Kappa test to verify inter-rater reliability. The k-values of the BFSC and SEWSS were .35 and .80, respectively. The DFUAS was reliable with an intra-class correlation coefficient (ICC) of .98. Only the DFUAS suggested a cutoff score (i.e., 12), and the area under the curve (AUC) was .90.
The Foot Assessment Form, BFSA, and 60-second Tool used a dichotomous response format (yes/no), whereas the other three tools used a Likert scale.
3. Contents of the Six Tools
The subcategories of the tools included dermatologic, vascular, neurological, musculoskeletal, and current wound/ulcer changes. The high-frequency items in each subcategory were: ulcer, previous ulcer, and nail and calluses in the dermatology category; pedal pulse in the vascular category; sensation in the neurological category; previous amputation in the musculoskeletal category; and infection in the current wound/ulcer category. Among them, ulcers, previous ulcers, nail and calluses, previous amputation, sensation, and infection were identified as the most frequent items. Table 3 summarizes the contents of the six tools.
DISCUSSION
In this current review, the Foot Assessment Form, BFSC, SEWSS, UKST, Screening for the High-Risk Diabetic Foot: A 60-Second Tool (2012), and the DFUAS were found to assess the risk factors of diabetic foot. These six tools were developed for the diagnosis, prediction, and evaluation of diabetic foot. However, no single tool achieves all three purposes of diagnosis, prediction, and evaluation.
Screening for the High-Risk Diabetic Foot: A 60-Second Tool [20] was designed to be used within one minute for a quick and systematic foot screening. It has the advantage of being simple and quick to use; however, as a weakness, it allows for nothing more than a simple distinction of the current state of the foot. The DFUAS [17], developed in 2016, also only enables a distinction of the current state of foot complications. Although it is important to detect and manage risk factors early to prevent diabetic foot ulcers [9], six assessment tools have only been applied after the impairment has already occurred. Especially four tools (the Foot Assessment Form, BFSC, SEWSS and UKST) were used only in patients with diabetic foot complications.
The sample sizes for these six tools ranged from 52 to 1,266 patients. The number of target subjects for the Foot Assessment Form and DFUAS were less than 70. Tools that were developed with a small number of participants have limitations in their use because they have not satisfied the normal distribution. Furthermore, only one tool (the DFUAS) presented a cutoff score and psychometric properties in terms of reliability and validity. Two tools (the Foot Assessment Form and the UKST) did not evaluate psychometric properties (validity and reliability).
The response format varied for each tool. Three of the six tools used a dichotomous response format (yes/no questions), which indicated high risk when the answer was yes. A dichotomous classification has the weakness of enabling nothing more than a superficial assessment due to the difficulty in precisely assessing the current state [21]. This finding was consistent with a study [22] that pointed out that healthcare providers may overlook the risk of diabetic foot complications occurring in diabetic patients, which often leads to a missed window of time that is critical for treatment. Therefore, the tools that include a variety of information in terms of diabetic foot risk factors and a more detailed scoring system should be developed. Risk factors for diabetic foot complications include nerve damage and peripheral vascular diseases, and behavioral factors are secondary to infection, which results in amputation [23].
As such, various factors are related to diabetic foot, the most assessed items for each tool were foot ulcers, previous ulcers, nails and calluses, previous amputation, sensation, and infection, which is almost in line with the guidelines for the assessment of diabetic foot complications by the American Diabetes Association [23]. The advantage of all tools is that they can be used to assess patients easily and quickly, perform appropriate interventions, and prevent patients from unnecessary hospitalization or amputation through early diagnosis. Similar to skin wound assessment tools such as the PSST and PUSH, four tools focused on the physical signs and symptoms in the patient’s current status. Only the BFSC and UKST included items that could assess educational needs and foot care capacities. The most reviewed tool did not reflect the behavioral factors for diabetic foot self-care. In clinical and community healthcare settings, diabetes educators have emphasized foot care to all patients with DM [24]. New guidelines published by the ADA in 2019 stated that “all patients with diabetes and their families should be provided general education about appropriate foot management and monitoring on a daily basis for surveillance of early foot problems”[24].
Based on this current review for diabetic foot assessment, various evaluations should be added to the existing tools, such as foot care practice and heath behaviors (e.g., smoking). Moreover, tools that contain diabetes self-management, including preventive behavioral factors as well as physical risk symptoms and signs, should be required. This study is significant because previously developed assessment tools for diabetic foot complications were systemically examined. By determining the characteristics and usefulness of each tool, the results of this study can guide the future development of assessment tools for foot complications.
CONCLUSION
Accurate diabetic foot assessment is important to determine high-risk individuals, as well as to prevent existing ulcers from worsening and requiring amputation. Healthcare providers should educate patients with DM on appropriate foot care and perform foot inspections at every visit, regardless of their level of risk for foot ulcers and amputations. In future study, multidimensional assessment tools including physical risk factors as well as behavioral risk factors related to diabetic foot complications should be developed based on the findings from this integrative review.