Factors Influencing the Subjective Health Status of Men with Insulin-treated Type 2 Diabetes Mellitus: A Secondary Analysis Using Quantile Regression Analysis
Article information
Abstract
Purpose
The aim of this study was to identify the factors associated with the subjective health status by level in men with type 2 diabetes mellitus (T2DM) receiving insulin treatments.
Methods
This study was a secondary analysis. A total of 120 male outpatients with insulin-treated T2DM completed in a questionnaire from July to November 2019, and results were analyzed using multiple linear and quantile regression to determine factors related to subjective health status. The 10th, 25th, 50th, 75th, and 90th conditional quantiles were considered with the aim of identifying different factors that contributed to subjective health status.
Results
Subjective health status was measured by the EuroQol visual analog scale, and its mean score was 61.29±19.00 points out of 100. Through ordinary least squares analysis, family support, knowledge, self-care, and psychological insulin resistance explained 57.2% of the variance in subjective health status. Through quantile regression analysis, family support and knowledge were identified as factors significantly related factors for all percentiles, and self-care and psychological insulin resistance were the significant factors for the 50th, 75th, and 90th percentiles.
Conclusion
The results of this study highlight the importance of the subjective health status of men with T2DM receiving insulin treatment, especially healthcare professionals looking for more effective intervention methods. Strategies that take into consideration various factors that explain an individual's subjective health status have the potential to improve patient health.
INTRODUCTION
Diabetes affects more men than women worldwide, and as a lifestyle-related disease, gender difference is important in the awareness, diagnosis, and treatment of type 2 diabetes mellitus (T2DM), and men with T2DM were more influenced by gender-socioeconomic status interactions than women [1]. For example, men with T2DM have a higher prevalence of smoking and alcohol consumption, which predisposes them to a broader range of health risks and may contribute to men having a lower life expectancy than women [2]. While men patients are prone to having diabetes complications such as diabetic foot syndrome, and diabetic nephropathy [1], women patients are more likely to show compliance and better adherence [3]. Furthermore, one Korean study acknowledged that men patients had negative perceptions of insulin treatment, whereas women patients had both negative and positive perceptions of their insulin use [3].
Men and women have different levels of life satisfaction [4], and subjective health status is a measure of perceived health that has proven to be a valid predictor of an individual's future medical composition [5]. Subjective health status is strongly associated with self-management in patients with T2DM [6], and efforts have increased to better understand health-related quality of life among patients with T2DM and its related factors, which are essential to better diabetes management [7]. Also, subjective health status is associated with glucose metabolism and the pathogenesis of T2DM [8] and studies have revealed gender disparities in this association [8,9], with men patients being known to have poor adherence to food regimens and medicines [2]. However, patients with DM tend to rate their health as poor [10]. Thus, it should concern health professionals.
Literature also showed that subjective health status is associated with the several factors including gender, family support [8,10], duration of diabetes, insulin therapy, and HbA1c [9] in diabetes patients. In addition, variables such as diabetes knowledge [11], self-care [6,12], and attitude toward self-care [13] are known to be significantly related to the subjective health status and quality of life of patients with T2DM.
In our previous path model study of subjective health status in patients with T2DM undergoing insulin treatment, we found that psychosocial variables - including diabetes knowledge, psychological insulin resistance, family support for diabetes management, and diabetes self-care ac-tivities - had a direct impact on subjective health status, as did HbA1c levels. On the other hand, diabetes management self-efficacy was found to exert an indirect effect [14].
However, it remains to be seen how these variables will relate to different levels of subjective health status. Understanding the relevance of these variables across different levels of subjective health status can guide health professionals in implementing more effective interventions, especially for those with low subjective health status who need more attention. In doing so, we can help insulin-treated men with T2DM manage their disease in a more personalized manner.
To this end, we only selected men patients’ data from our original study to apply a quantile regression analysis to investigate factors associated with subjective health status. Ordinary Least Square (OLS) regression focuses on the mean and is a standard method of estimating how independent variables relate to changes in a dependent variable. In reality, it is common that the relationship between variables can change at different points in a distribution. Quantile regression is a better analytic technique suited for our study because it can overcome some of the limitations of conventional methods especially when the research aims to explore the relationship at various locations along the distribution [15]. This study aimed to evaluate the subjective health status of insulin-treated men with T2DM and determine the related variables using the quantile regression analysis. We aim to provide new insight by examining the associations between study variables at different levels of subjective health status to help health professionals implement interventions for those with lower subjective health status.
The specific purposes of this study are as follows: First, determine the general characteristics and level of research variables in men with T2DM. Second, identify differences in subjective health status according to the general characteristics of men with T2DM. Third, determine the relationship between research variables. And fourth, identify factors related to each quantile of subjective health status.
METHODS
1. Design
This study was a secondary analysis using research data obtained from examining the health status of men with T2DM undergoing insulin treatments. The prior study employed a cross-sectional survey design [14].
2. Participants
In a parental study [14], convenience sampling was used to recruit individuals for the study. The inclusion criteria were as follows: (i) over nineteen years old, (ii) received a diagnosis of T2DM while undergoing insulin treatments for a minimum of six months, (iii) able to understand the study's aim and willing to participate, and (iv) able to understand the questionnaire contents. 204 subjects from Jeonbuk National University Hospital's metabolic endo-crinology department in Korea were invited to participate, but 11 participants were excluded due to incomplete data. The criterion for incomplete answered responses was that more than 50% of the questionnaire was blank. The total population for the parent study comprised 193 participants, both men and women. However, for the purposes of this research, we utilized data exclusively from 120 men participants. The appropriate sample size for quantile regression is 100 or more [16].
3. Measurements
1) Demographic and disease-related characteristics
Participants’ general characteristics including gender, age, education level, marital status, and cohabiting (i.e. alone, or with spouse or family) were collected. And disease-related characteristics including weight, height, time since diabetes diagnosis, duration of insulin treatment, and history of hospitalizations due to diabetes and diabetes-related complications were also collected. Most recent HbA1c levels at the time of questionnaire completion were recovered from electronic medical records.
2) Knowledge
The Korean version of the Michigan Diabetes Research Center's Brief Diabetes Knowledge Test [17,18] was used to measure the participants’ knowledge regarding diabetes and insulin treatments. This scale consists of 23 mul-tiple-choice questions and is divided into two sections. The 14-item general knowledge component of the test is appropriate for people with type 2 diabetes. An additional 9 items comprise the insulin use subscale, which is suited for people with type 2 diabetes who use insulin; participants choose one of four possible responses for each question. Each correct answer is awarded one point, and an in-correct answer is awarded zero points. The total score ranged from 0 to 23, with 23 reflecting the highest level of diabetes knowledge and 0 reflecting the lowest. At the time of development of the Korean version, Cronbach's ⍺ was .72∼.82, and in this study, Kuder-Richardson Formula 20 was .71 and .70, respectively.
3) Psychological insulin resistance
Psychological Insulin Resistance Scale for Korean Diabetes [19] was used. This scale includes 18 items with a five-point Likert scale. It is differentiated by 14 cognitive-psychological items and 4 support-related items. A higher score indicates greater levels of psychological insulin resistance. At the time of development of the Korean version, the calculated Cronbach's ⍺, based on the exploratory factor analysis data and confirmatory factor analysis data, were .91 and .87, respectively. In this study, Cronbach's ⍺ was .90 and .88, respectively.
4) Family support
The Korean version of the Diabetes Family Behavior Checklist II [20,21] was used to measure family support. This version features 10 items with a four-point Likert scale and a higher score indicates greater levels of perceived familial support. At the time of development of the Korean version, Cronbach's ⍺ was .85, and Cronbach's ⍺ in this study was .92.
5) Self-efficacy
The Korean version of the Diabetes Self-Efficacy Scale [22,23] was used to measure self-efficacy. The Korean version consists of 18 items with a six-point Likert scale and a higher score indicates greater self-efficacy. At the time of development of the Korean version, Cronbach's ⍺ was .89, and Cronbach's ⍺ in this study was .89.
6) Self-care
The Korean version of the Summary of Diabetes Self-Care Activities [24,25] was used to measure self-care. We employed 9 items on a scale of 0∼7, indicating the number of days in a week where respondents perform self-care activities. Higher scores indicate better performance on self-care in diet, physical activity and exercise, blood sugar testing, and medication. At the time of development of the Korean version, Cronbach's ⍺ was .71, and Cronbach's ⍺ in this study was .72.
7) Subjective health status
The Korean version of the EuroQol visual analog scale (EQ-VAS) from the EQ-5D [26] was used to measure subjective health status. In this scale, participants rate their general health status on a scale from 0 (worst imaginable health state) to 100 (best imaginable health state).
4. Ethical Considerations
This study was endorsed by the Research Ethics Committee of Jeonbuk National University's (IRB No.: JBNU 2021-07-021) Institutional Review Board for a secondary analysis. In parental study, we performed all study methods in compliance with the Helsinki Declaration. Preceding data collection, the methods and aim of the research were described to the participants and their consent was obtained; additionally, patients were advised of their right to discontinue participation whenever and were understood their anonymity and the non-disclosure of their responses. All participants who were included in the study were obliged to present their informed consent in writing.
5. Data Collection
In the parental study [14], data were collected between July 22nd and November 1st, 2019, from the metabolic en-docrinology department of Jeonbuk National University Hospital in Korea. Participation was elective, and all of the voluntary participants were encouraged to finish the questionnaire. The structured questionnaires were self-administered, and the questionnaires were completed in 20 to 30 minutes on average. The researchers assigned a serial number to each participant and stored the data in a secure box to ensure confidentiality.
6. Data Analysis
All statistical analyses were conducted using Stata version 16.0 (StataCorp LP). Descriptive statistical analysis was performed for the participant's characteristics and study variables. Differences in subjective health status de-pending on the participants’ characteristics were analyzed by using an independent t-test, a one-way ANOVA, and a Scheffé test for the post hoc analysis. The relationships among the study variables were tested by using Pearson correlation coefficients. Multiple linear regression analysis was performed to identify factors related to subjective health status. Quantile regression analysis was performed to identify related factors according to subjective health status levels. All regression analyses were adjusted for demographic characteristics (age, gender, education level, and living status) and disease-related variables (time since diabetes diagnosis and duration of insulin treatment). Two-tailed p<.05 was considered statistically significant and 95% confidence intervals (CI) were used in this study.
RESULTS
1. Participants’ Characteristics and Differences in the Subjective Health Status according to the Characteristics
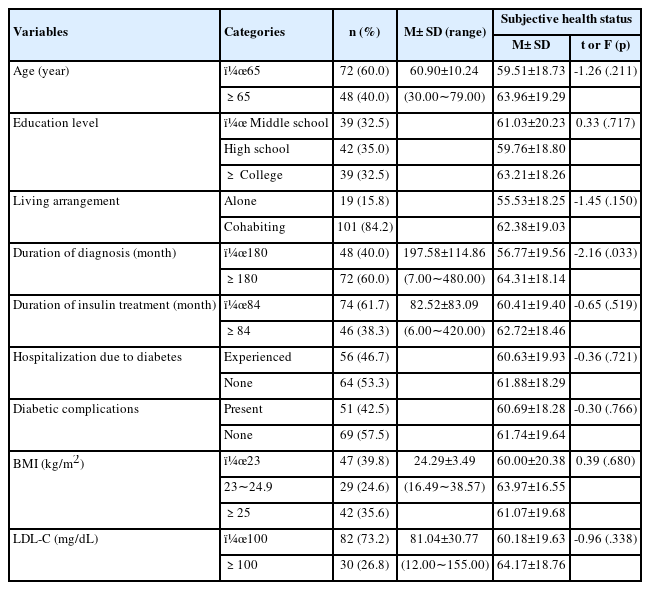
The general and disease-related characteristics of our participants are displayed in Table 1. Most of the participants were less than 65 (60.0%), and the participants’ mean age was 60.9±10.24 years. Education levels were evenly distributed and 84.2% of participants lived with spouses or other family members. The mean time since T2DM diagnosis was 16.5±9.57 years, with a mean duration of insulin treatments measuring 6.9±6.92 years. 53.3% of participants had no experience of hospitalization due to T2DM, with 57.5% not having a history of diabetes complications. 39.8% of our participants showed a body mass in-dex of less than 23. And low-density lipoprotein cholester-ol levels were below 100 in 73.2% of our participants. In addition, based on the characteristics of the participants, there was no significant difference in subjective health status (Table 1).
2. Descriptive Characteristics and Normality and Multi-collinearity of observed variables
The mean scores for knowledge, psychological insulin resistance, family support, self-efficacy, self-care, and HbA1c were 15.52±3.82, 46.99±12.63, 27.34±9.49, 72.08±20.05, 33.12±7.37, and 8.23±1.58 respectively. The mean score for subjective health status was 61.29±19.00 (Table 2). Pearson correlation coefficients were used to examine the multi-collinearity of study variables with subjective health status (Table 3).
3. Quantile Regression and Multiple Linear Regression for Subjective Health Status
The result of quantile regression and multiple linear regression analysis for subjective health status and the possible related factors are presented in Table 4 and Figure 1. In the OLS analysis, family support (B=0.58, β=.29, p <.001), knowledge (B=1.38, β=.28, p<.001), self-care (B=0.74, β=.29, p< .001), and psychological insulin resistance (B=-0.26, β=-.18, p=.010) were evaluated to be significant related factors of subjective health status.

Quantile Regression and Multiple Linear Regression Analysis of the Factors Influencing Subjective Health Status (N=120)
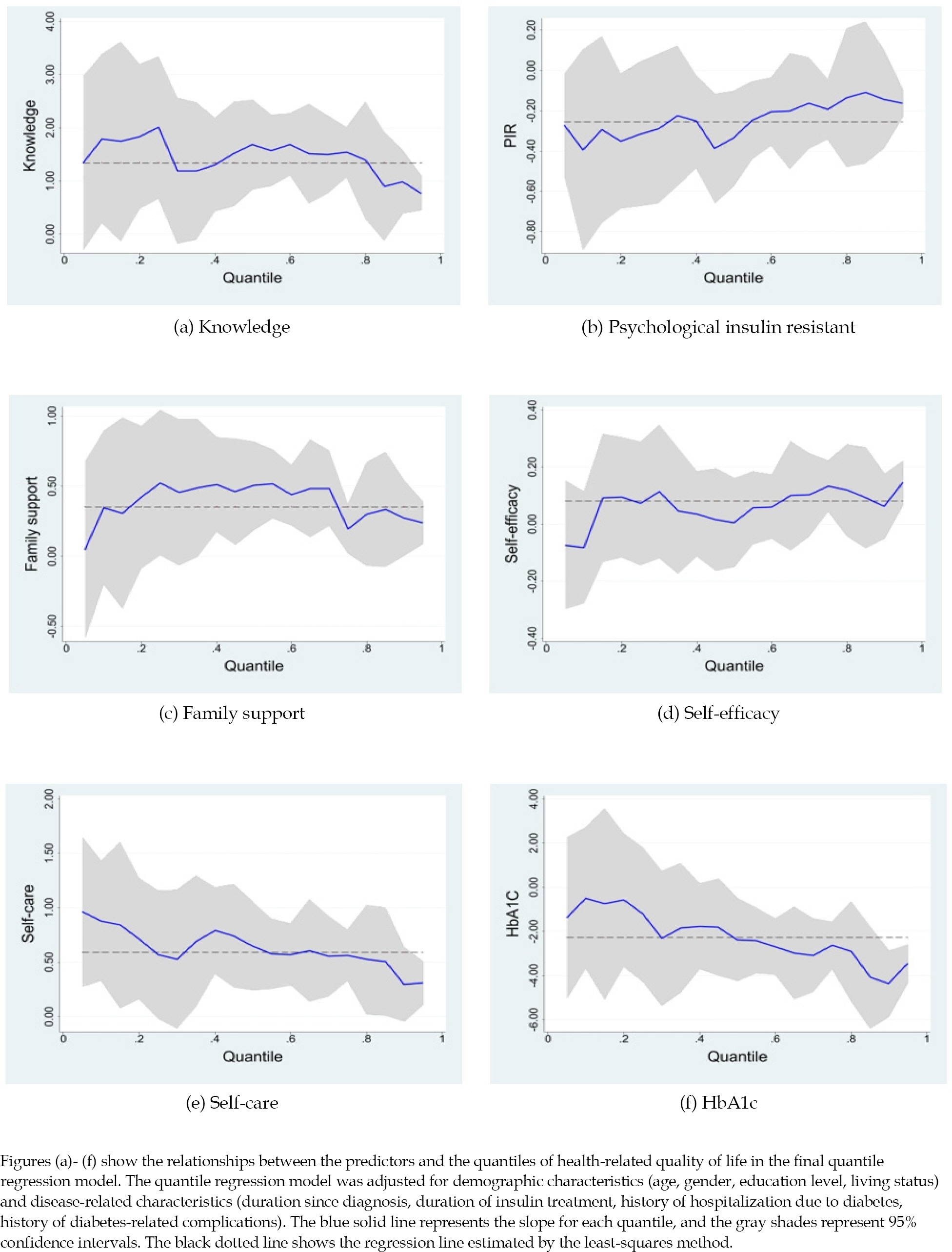
Association between knowledge, psychological insulin resistance, family support, self-efficacy, self-care, and HbA1c.
In the quantile regression analysis, family support (B=0.90, p<.001) and knowledge (B=1.15, p=.048) were significant related factors of subjective health status at the 10th percentile. At the 25th percentile, family support (B=0.77, p<.001), knowledge (B=1.42, p=.005), and HbA1c (B=-2.74, p=.038) were significant related factors of subjective health status. At the 50th percentile, family support (B=0.67, p<.001), knowledge (B=1.67, p<.001), psychological insulin resistance (B=-0.40, p=.001), and self-care (B=0.68, p=.005) were significant related factors. At the 75th percentile, self-care (B=0.61, p=.011), family support (B=0.40, p =.012), knowledge (B=0.99, p =.015), and psychological insulin resistance (B=-0.30, p=.016) were significant related factors of subjective health status. Finally, self-care (B=0.59, p<.001), psychological insulin resistance (B=-0.26, p=.002), knowledge (B=0.75, p=.007), family support (B=0.29, p=.009), duration of diagnosis (B=5.07, p=.011), and HbA1c (B=-1.49, p=.039) were significant at the 90th percentile of subjective health status.
DISCUSSION
There is growing proof of clinically significant sex and gender disparities along with an increase in T2DM and related comorbidities [1]. In the present study, the mean EQ-VAS score of men patients was 61.29, which was considerably low compared to other results of T2DM patients measured by the same tools. For example, a study conducted between 2007∼2009 (KNHANES) had an EQ-VAS score of 71.94 [27], and the PANORAMA, cross-sectional T2DM study in nine countries of Europe had an EQ-VAS score of 70.55 [28]. The relatively lower subjective health status of our study's participants can be attributed to them undergoing insulin treatment. This is supported by a previous study that found men patients have negative perceptions of insulin treatments [3]. However, other studies with T2DM suggest that men's EQ-VAS health status scores were better than women's [28,29]. Thus, research comparing the subjective health condition of patients with T2DM undergoing insulin treatment by gender is required. In addition, health providers must pay close attention to the low EQ-VAS score of men patients receiving insulin treatment.
To improve patients’ subjective health status, considering all related variables is important. Most studies involving the subjective health of patients with T2DM were con-cerned with socio-demographic variables (e.g., age, gender, marital status, occupation, and level of education, etc.), disease-related variables (e.g., duration of diabetes, number of medications, presence of complications, insulin therapy, or HbA1c, etc.) or psychosocial variables (e.g., attitudes, stress or depression, etc.) [9,13,27,29,30]. This study provides evidence that variables such as family support, knowledge, self-care, and psychological insulin resistance are significant predictors of subjective health status among insulin-treated men patients through OLS analysis.
In the quantitative regression analysis, it was found that family support and knowledge were significant variables at all subjective health status levels and that these were the only variables that were significant for participants with low subjective health status (at the 10th and 25th percentiles). Family members are important sources of both instrumental and emotional support to patients with T2DM [31]. A study of Korean immigrants with T2DM reported that Korean men received and appeared to utilize family support more effectively than women, and they rely heav-ily on their spouses for family support, whereas women rely on their network of friends and other relations [32]. Our result adds evidence of the importance of family support for insulin-treated men with T2DM and suggests fortifying it, especially for those with low subjective health.
There are mixed results regarding the association of diabetes knowledge with subjective health status. In some instances, better diabetes knowledge has been linked to a higher quality of life [11], while in others, it appeared to have no impact [13]. Nevertheless, our result should be interpreted in line with the results of a recent study in which an educational program increased diabetes patients’ level of diabetes knowledge and improved adherence and glycemic control to enhance health-related quality of life [33]. This suggests providing consistent education about disease progress and self-care to men with T2DM will benefit their subjective well-being as well as clinical outcomes. And also, healthcare professionals should work with not only men patients but also with family members including their spouses in designing education programs.
Self-care was an important variable at the 50th percentile and above of our participants in quantile regression analysis and OLS, meaning adherence to self-care influen-ces, especially men patients with better subjective health status. This result supports the result of previous studies that healthy lifestyle behavior had a relation with self-rated health among Chinese men with T2DM [6]. Nevertheless, it is worth noting that Asian men are less compliant with physicians’ recommendations than women patients [3]. Thus, healthcare professionals keep endeavoring to enhance self-care when dealing with men patients with low subjective health status.
Lastly, psychological insulin resistance was another important variable at the 50th percentile and above of our participants in quantile regression analysis and OLS. Psychological insulin resistance was also an important factor for participants with better subjective health status. Negative perceptions of insulin treatment were found in men patients [3]. Addressing and managing psychological insulin resistance can benefit the health outcomes of T2DM patients [22]. Reasonably, a cognitive program designed with elements of education and family involvement may significantly improve health outcomes for insulin treated T2DM men with low subjective health status.
Besides the aforementioned variables, variables such as duration of diagnosis and HbA1C were associated with the subjective health status of the participants with high subjective health status. This finding validates a prior study's finding that the HbA1c level significantly was associated with the EQ-VAS score [34]. Also, it is worth no note that multidisciplinary team management led by a community nurse demonstrated a reduction in HbA1c and an increase in quality of life during a 24-month period [35], for it suggests healthcare professionals including nurses may play an important role to promote subjective health and clinical outcomes of increasing men with T2DM. However, this finding contradicts the finding that the longer the duration of diabetes, the lower the VAS score [29], as a duration of 180 months or more was positively associated with subjective health status in our study. More research to investigate diabetes duration and subjective health status will be needed in the future.
This study employed multiple linear regression and quantile regression analysis to examine the related factors for subjective health status in insulin-treated men patients with T2DM. In our study, quantile regression allows us to examine individuals with low subjective health status and provides a guide to developing specific interventions to effectively promote their subjective health and clinical outcomes by revealing the related factors at different levels of subjective health status. This is important because related factors of patients with low levels of subjective health status, which we identified in this study as family support, knowledge, self-care, and psychological insulin resistance are amenable to change while demographic or disease-related variables are not.
Our study is not without its limitations. The results of this study should be interpreted carefully. Our prior study was a cross-sectional study making use of convenience sampling that cannot establish a causal relationship between independent variables and subjective health status. Also, selection bias may limit the generalization of the findings. Since we recruited participants from a university hospital, selection bias could also be present in this study. Those who agreed to participate in the study may have more interest in their subjective health status than those who did not. In addition, as we only analyzed responses from men, it is difficult to compare our findings with those of previous studies or women. Finally, a comparison of subjective health status levels between this study and the others should be done with precaution as we only used EQ-VAS from EQ-5D. Longitudinal studies or experimen-tal studies measuring subjective health status with both EQ-5D Index and EQ-VAS may be needed to confirm cau-sality and examine the related factors over time and their effects on subjective health status.
Despite these limitations, this study has several clinical implications for healthcare professionals. First, our study shows that insulin-treated men with T2DM have low levels of subjective health status, which should be a concern for healthcare professionals. Second, our study provides information that family support and diabetes knowledge are important factors for insulin treated T2DM men with low subjective health status. Third, our findings can guide healthcare professionals in designing and implementing intervention programs that include family support and diabetes education for insulin-treated men with T2DM, in particular for those with low subjective health status.
CONCLUSION
The results showed that insulin-treated men with T2DM have poor subjective health status and need attention and interventions from healthcare professionals. Although family support, diabetes knowledge, self-care, and psychological insulin resistance were found to be significant factors related to subjective health status in OLS, patients in different conditional quantiles were associated with other variables. These findings suggest a need to assess subjective health status to provide more personalized interventions for insulin-treated men with T2DM with different levels of subjective health status. Structured intervention programs incorporating family support and education, especially for T2DM men with poor subjective health status, have the potential to significantly improve their ability to manage their physical condition and, as a result, their quality of life.
Notes
CONFLICTS OF INTEREST
Hye Young Kim has been editor-in-chief of the Journal of Korean Academy of Fundamentals of Nursing since January 2022. She was not involved in the review process of this manuscript. Other-wise, there was no conflict of interest
AUTHORSHIP
Study conception and design acquisition - Lee KS, Kim HJ, Kim YM, and Kim HY; data collection - Lee, KS; data analysis and inter-pretation - Lee KS; Kim HJ, and Kim YM; drafting and revision of the manuscript - Lee, KS, Kim HJ, Kim YM and Kim HY.
DATA AVAILABILITY
The data that support the findings of this study are available from the corresponding author upon reasonable request.