Effects of Auricular Acupressure Therapy on Psychological Factors, Sleep Quality, and Salivary Cortisol Levels in South Korean Older Adults in the Community: A Single-blind, Randomized Controlled Trial
Article information
Abstract
Purpose
This study aimed to investigate the effects of auricular acupressure (AA) therapy on psychological factors, sleep quality, and salivary cortisol levels in community-dwelling older adults.
Methods
This was a single-blind, randomized, placebo-controlled comparative pretest-posttest study that applied AA for three weeks. The experimental group received AA on the shenmen, sympathetic, subcortical, and adrenal areas, while the control group received acupuncture in four areas along the helix. Nineteen participants were assigned to the experimental group and 21 to the control group. All participants were community-dwelling seniors aged 65 years or older who had an Insomnia Severity Index score of 8 or higher and experienced psychological stress. Depression, anxiety, and stress were measured using the Korean version of the Depression Anxiety Stress Scale for psychological factors, and the Korean version of the Pittsburgh Sleep Quality Index and morning salivary cortisol levels were measured to evaluate sleep quality.
Results
Statistically significant differences were observed between the groups for depression (t=5.56, p<.001), anxiety (t=3.53, p=.001), and stress (t=3.55, p=.001). The PSQI (t=4.72, p<.001) and salivary cortisol levels (z=-4.21, p<.001) showed statistically significant differences between the groups.
Conclusion
AA demonstrated its effectiveness as an intervention for addressing complex symptoms in community-dwelling older adults. It was found to alleviate depression, anxiety, and stress, enhance sleep quality, and reduce salivary cortisol levels.
INTRODUCTION
The population is aging rapidly worldwide; the elderly population was 12.0% in 2015 but is predicted to double to 22.0% by 2050 [1]. In 2020, Korea's life expectancy at birth is 83.5 years, but the ‘healthy life years’ is 73.1 years [2]. Recently, the concept of Aging in Place (AIP), which delays admission to a facility as much as possible while maintaining an independent life at home and in the community by extending the healthy lifespan, has been supported [3]. Therefore, nursing interventions for continuous care and health maintenance are required so that the elderly can lead healthy lives. In general, aging is associated with various factors that cause stress, such as health problems such as reduced functional ability, chronic diseases, frailty, and pain, and events such as loss of socioeconomic status due to spousal bereavement and retirement [4,5]. In elderly individuals with depression and anxiety, the prevalence of frailty is higher [6], and elderly individuals with severe stress have a higher mortality risk [4]. In 2021, the number of anxiety disorder patients in Korea was the highest at 18.5% in their 60s and older, and the elderly and depressed patients also increased by 14.2% compared to 2017 [7].
Sleep disorders in the elderly increase the prevalence of multimorbidity by 55.0-98.0% in combination with other symptoms, such as depression and stress [8,9]. According to the Korea National Health and Nutrition Examination Survey, stress is a significant factor in the sleep of the elderly in Korea, and older adults with high stress have a higher risk of poor sleep [10], depression, and anxiety in the elderly are also closely related to sleep disorders [8,11]. In particular, depression in the elderly is the factor most related to suicidal ideation [12], and the suicide rate of the elderly in Korea is 17.2 per 100,000 population, ranking first among Organization for Economic Co-operation and Development countries [13]. Therefore, there is a need for a continuous intervention method that can be easily applied with fewer side effects to alleviate psychological factors in the elderly and improve their sleep quality.
Depressive disorders, anxiety, and stress are activated by the stress axis and can be seen as similar symptoms [14,15]. Cortisol, immunoglobulin A, lysozyme, melatonin, and ⍺-amylase are salivary biomarkers for measuring depression, anxiety, and stress, and among them, cortisol is the most valuable potential salivary marker for stress [9,14]. Changes in cortisol concentration are strongly related to human psychological conditions, such as stress, anxiety, and depression [9,14,16]. Elderly individuals who engage in high levels of physical activity experience an increase in salivary cortisol levels when exposed to stress [17]. When depression and suicidal thoughts in the elderly decreased, cortisol levels also decreased [9]. When stress decreases in middle-aged women, cortisol levels also decrease [18], so cortisol can be considered an indicator of psychological factor levels.
In AA therapy, a complementary and alternative therapy, the whole human body corresponds to a specific part of the ear, and the nervous system cause a reaction transmitted to the neuron to reduce or disappear symptoms [19]. The corresponding area of the ear is stimulated with seeds, beads, magnets, etc., in a non-invasive manner, and acupoints relieve symptoms and have a therapeutic effect, preventing serious medical conditions [19,20]. In addition, there is less pain and fewer side effects during the procedure; the procedure is simple and can be performed simply regardless of location [19]. In 1990, the World Health Organization (WHO) recognized the final 91 auricular acupoints as standardized for the anatomical structure of the ear and standard transfusions, which have been used until now [19,20]. In the literature on AA therapy for the elderly, there are studies on the effects of musculoskeletal pain, depression, and sleep in the elderly living in facilities [21] and studies on shoulder pain and joint range of motion [22]. A study on the effects of sleep and pain in the elderly with arthritis in a nursing home [23]. A large number of studies have been conducted on the effects of chronic pain and sleep on elderly people living in nursing homes or facilities. While there are studies examining the sleep effects among elderly individuals visiting senior welfare facilities [24,25] the close relationship between psychological factors and sleep in the elderly is noteworthy, and therefore it is necessary to verify the effectiveness of AA therapy to provide psychological stability to the elderly and improve all complex symptoms of sleep quality. Therefore, this study aimed to confirm the effect of 3-week AA therapy on psychological factors, sleep quality, and salivary cortisol levels by applying a single-blind, randomized assignment to elderly people in the community.
METHODS
1. Design
This was a single-blind, randomized, placebo-controlled comparative test study to investigate the effects of AA therapy using vaccaria seeds on psychological factors, sleep quality, and salivary cortisol levels in elderly individuals.
2. Participants
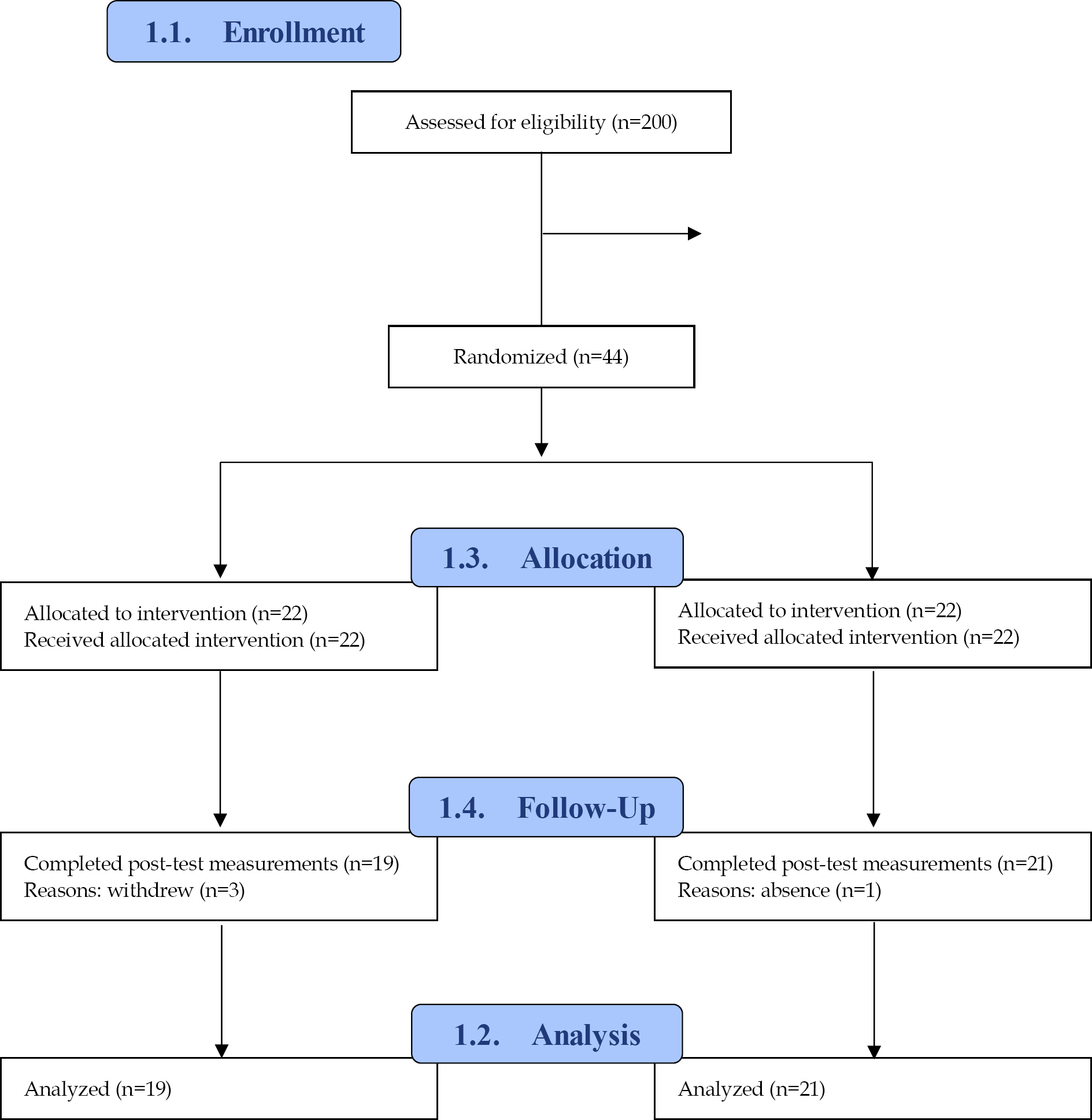
The study period was from October 2022 to March 2023. Among the elderly visiting the Seongnam city senior center, subjects who met the selection criteria and voluntarily agreed to participate in the study were randomly assigned. The inclusion criteria were aged 65 years or older, ISI (Insomnia Severity Index) 8 points or higher [26] psychological stress [27], and no inflammatory lesions or trauma to the ear. As for the exclusion criteria, those receiving other complementary and alternative therapies using acupuncture or auricular pressure and those taking sleeping pills for insomnia were excluded. The G*Power 3.1.9 program was used to calculate the sample size, and based on the study of Cha et al. [18], assuming that the effect difference between the two groups was 2.04 and the standard deviation of the two groups was σ1 2.94 σ2 1.65, The effect size calculated in a single test for the difference of significance level (⍺) .05 and power .80 was .85, and as a result of the calculation, the number of study subjects was tested to be 18 in the experimental group and 18 in the control group. In this study, a dropout rate of 15.0% was calculated, and thus, 22 participants were selected for the experimental group and 22 participants for the control group. For random assignment, a random number table generated by the Random Allocation Software Version 2.0.0 program was used. As for the subjects, a total of 200 elderly people registered at the senior center were notified of the recruitment of the study by text message, and among them, 102 subjects who did not meet the selection criteria and 54 persons who refused to participate in the study were excluded, 156 persons were excluded, and a total of 44 persons were registered. Twenty-two people were randomly assigned to the experimental group and the control group. Three people withdrew consent from the experimental group, and one from the control group was excluded for personal reasons (Figure 1).
3. Measurements
1) Psychological factors
Psychological factors were measured using the DASS-21 for depression, anxiety, and stress [27]. The Korean version of the Depression Anxiety Stress Scale (K-DASS-21) was used [28]. Three subdomains on depression, anxiety, and stress, the tool has a total of 21 items, composed of 7 items in each domain. The score range for each sub-domain was divided into five levels: normal, mild, moderate, severe, and extremely severe. The normal ranges of depression, anxiety, and stress, respectively, is 0∼4, 0∼3, 0∼7 points, mild ranges are 5∼6, 4∼5, 8∼9 points, and moderate–7∼10 points, 6∼7 points. Points, 10∼12 points, severe are 11-13 points, 8∼9 points, 13∼16 points, and extremely severe, 14+, 10+, 17+. Higher scores indicate greater levels of depression, anxiety, and stress. At the time of tool development, Cronbach's ⍺ was .88 for depression, .82 for anxiety, and .90 for stress, and in this study, Cronbach's ⍺ was .85 for depression, .71 for anxiety, and .81 for stress.
2) Sleep quality
Sleep quality was measured using the Pittsburgh Sleep Quality Index (PSQI) [29]. The Korean version of the PSQI (K-PSQI) was used [30]. The PSQI contains 19 items and generates seven components: subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbance, use of sleeping medication, and daytime dysfunction during the past month. The scores for each component ranged from 0 to 3, and the sum of the global scores ranged from 0 to 21. Higher global scores are associated with lower sleep quality. A score of 5 or less was classified as a good sleeper, and a score of 5 or more was classified as a poor sleeper [29]. Cronbach's ⍺ of the tool at the time of development was .83, and Cronbach's ⍺ of this study was .81.
3) Salivary cortisol levels
Cortisol levels are regulated through the HPA axis (hypothalamus-pituitary-adrenal neuroendocrine) and vary in a circadian rhythm, being highest at around 6 AM and lowest around 4 PM [31]. In a previous study conducted with older adults, stress measurement was carried out using morning salivary samples between 8 to 10 AM [32], with the timing adjusted to be between 9 to 10 AM to minimize errors due to hormonal fluctuations. Between 9:00 and 10:00, a salivary cortisol enzyme-linked immunoassay (EIA) kit collected approximately 2 ml of saliva from the sublingual area. Morning cortisol level was used to measure the stress of study participants in this study, and the normal range is 0.09 to 1.55 ug/dL [31]. The higher the respondent's score, the higher their level of stress.
4. Rationale for AA selection
In this study, the acupressure points were stimulated by relaxation effects. shenmen and sympathetic points are ‘ master points’ [33]. The shenmen point lowers stress and anxiety and calms the mind. The sympathetic point relieves excitement and stimulates the autonomic nervous system to balance [20]. The subcortex corresponds to the human brain [19,20] and effectively reduces anxiety, making it effective for insomnia [20,33]. The adrenal gland induces calmness, reduces anxiety, and regulates cortisol secretion [32].
5. Intervention
Both the experimental group and the control group completed the ISI questionnaire, and if they met the inclusion criteria, the K-DASS and K-PSQI tools were administered as a pre-survey. Salivary cortisol was measured to assess physiological indicators after the questionnaire survey. To prevent the diffusion of treatment, the experimental group visited at 9 am, and the control group at 10 am; the rooms visited by the experimental and control groups were different. Post-investigation was conducted similarly. The AA therapy took place within the meeting room and basic physical fitness measurement room located at the senior center. AA therapy was conducted by a researcher with 12 years clinical experience as a nurse in hospital, who had completed specialized training courses and obtained certification in AA therapy from the Korean Society of Complementary and alternative therapy. The AA therapy intervention used in this study was based on the ear acupressure therapy taught by the Korean Society of Complementary and Alternative Nursing [19].
In this study, commercialized seed stickers made of small 1 mm rings were attached to four acupressure zones: shenmen, sympathesis, subcortex, and adrenal gland points (Figure 2). The placebo control group was applied to a helical site that was separated from the inner ear area at four points to maintain single blindness. Based on previous studies, the helical area was determined to be located in a clearly different area from the auricular pressure point in the experimental group, as it was far from the inner ear area [20,24]. The adequacy of the pressure position was assessed by an AA therapy expert from the Korea Complementary and Alternative Therapy Nurses Association. AA therapy was administered alternately to each ear every week after removing the auricular seal. The participants were instructed to apply acupressure using their thumb and forefinger three times a day - morning, noon, and evening - on the ear pressure area. They were advised to press the part where the seeds were attached with enough pressure to feel a slight tingling or slight discomfort. An auricular seal was applied for six days at a time, with auricular seal being removed on the 6th day of each session. This therapy was conducted six times a week for three weeks. Every week, the researchers visited the senior center on the scheduled application days to administer AA therapy to the study participants. If the auricular seal fell off, participants notified the researchers via text massages, and it was reattached the following day during a visit to the senior center.
6. Data Analysis
Analysis was performed using SPSS version 26.0. The general characteristics and homogeneity between the two groups before the experiment were analyzed using the percentage of data, mean and standard deviation, χ2 test, Fisher's exact test, and independent t-test. The normality of the dependent variable was assessed using the Shapiro-Wilk normality test. Differences in changes in psychological factors and sleep quality between the two groups were analyzed using an independent t-test. Cortisol did not satisfy the normal distribution, so non-parametric Mann-Whitney U test was used for analysis.
7. Ethical Considerations
This study was conducted after receiving IRB review and approval from Eulji University (Approval No. EU23-01). Only participants who voluntarily consented after being fully explained the purpose and procedure of the study and receiving an explanation and consent form were enrolled. After the study was completed, the participants were informed of the group to which they belonged, and if desired, AA therapy was administered in the same way as in the experimental group.
RESULTS
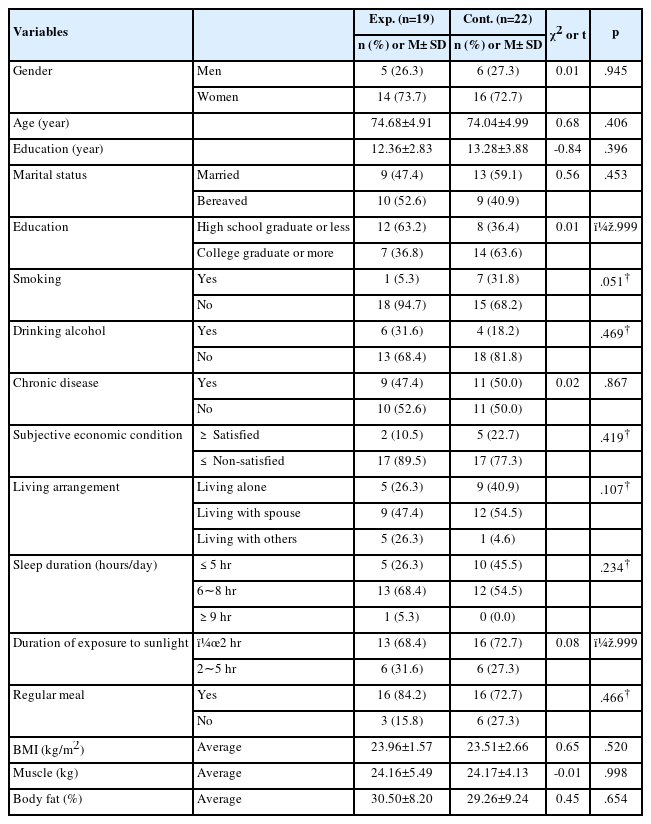
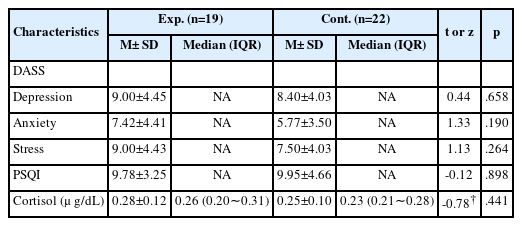
A total of 41 participants were included in this study:19 in the experimental group (5 males, 14 females) and 22 in the control group (6 men, 16 women). The mean age was 74.68±4.91 years in the experimental group and 74.04± 4.99 years in the control group (t=0.68, p=.406), and there was no statistically significant difference between the two groups in general characteristics such as education, marriage, smoking, drinking alcohol, and chronic diseases (Table 1). Table 2 presents the homogeneity test results for the dependent variables before the intervention. Depression (t=0.44, p=.658), anxiety (t=1.33, p=.190), stress (t=1.13, p=.264), PSQI (t=-0.12, p=.898), Salivary cortisol (z=-0.78, p=.441) showed no significant difference between the two groups, ensuring the homogeneity of the two groups. The effects of AA therapy are presented in Table 3.

Comparisons of Scores for Psychological Factors, PSQI, and Salivary Cortisol Levels between the Experimental and Control Groups
There were statistically significant differences in psychological factors such as depression (t=5.56, p<.001), anxiety (t=3.53, p=.001), and stress (t=3.55, p=.001). Depression in the experimental group decreased by 4.05 points, the degree of depression before the intervention was alleviated from moderate to mild, and anxiety decreased by 2.63 points and improved from moderate to mild. Stress decreased by 2.47 points from mild to normal levels. There was a statistically significant difference between the groups in PSQI (t=4.72, p<.001) and salivary cortisol levels (z=-4.21, p<.001). The PSQI decreased by 3.26 points in the experimental group, and salivary cortisol decreased by 0.05, proving that AA therapy effectively improves psychological factors, sleep quality, and changes in cortisol levels.
DISCUSSION
This study attempted to verify the effects of 3 weeks of AA therapy on psychological factors, sleep quality, and salivary cortisol levels in elderly individuals. The study's results showed that the psychological factors of the elderly in the community were moderate levels of depression and anxiety and mild levels of stress, but after the intervention, depression and anxiety decreased to mild levels, and stress was alleviated to normal levels.
In a study in which elderly residents living in a facility with musculoskeletal pain applied AA to 9 response points, including shenmen, kidney, heart occiput, and adrenal gland for 6 weeks, the depression score decreased by 7.08 points, supporting this study [21]. AA therapy was based on previous studies in which 4∼6 auricles were selected and applied for 5∼6 days, followed by a rest period of 1∼2 days and applied again [19,24]. In this study, four acupressure points, including the shenmen, were applied, and after six days of application, the elderly removed the sticker and maintained the application for six days in a cycle of 1 week. Chang's study used germanium otoliths because there are nine acupressure points [8], and it may be difficult for the elderly in the community to attach many of them. If the acupressure part fell off, it was considered that the accuracy of the AA therapy was reduced because the research participants or caregivers, not the researcher, directly applied it. In addition, there is a disadvantage in that the placebo effect could not be controlled by providing ear massages to the control group if desired. As a result of a study that applied AA therapy for 8 weeks to elderly people with hypertension and confirmed the effect on depression, anxiety, and stress, including physiological indicators, there was no significant difference between groups [34]. In this study, subjects with stress were selected as a selection criterion, and subjects with weak psychological factors were selected. However, in the study by Park et al. [34], only subjects with hypertension were selected, and auricular pressure points acted as acupressure points to lower blood pressure in the heart, kidneys, and occiput excluding shenmen, so it is considered that there is no effect on psychological factors. The shenmen, shympathesis is a commonly applied area [21,23] and has been proven effective in improving psychological stability. To date, previous studies on AA therapy have focused on the effects on sleep and pain in patients with arthritis living in nursing homes [23] and on musculoskeletal pain, depression, and sleep in elderly people living in facilities [21]. Self-care strategies are needed to enable older adults to live independently [3]. Therefore, this study is meaningful in that it proved that AA therapy could be used as a self-care therapy for the psychological stability of the elderly, targeting the elderly registered at a local senior center because they can live independently.
In this study, it was confirmed that the PSQI decreased by 3.26 points and was effective in improving the quality of sleep. The results of a study in which AA therapy was applied to a total of 9 places for 6 weeks for elderly people living in a nursing facility [21] and a study for elderly people with sleep disorders showed improved sleep [25], supporting this study. In addition, in a study targeting elderly people with sleep disorders with a PSQI score of 5 or more, the difference between the experimental group and the control group before and after PSQI intervention decreased by 7.62 points and 6.32 points, indicating that there was a difference within the group but no significant difference between the groups [24]. In the study by Lee [23], subjects were recruited at six senior citizen centers and welfare centers. In the homogeneity test between groups, only body mass index, disease, and smoking alcohol drinking were investigated, and the factors influencing sleep in the elderly such as marital status, presence of a spouse, education level, and exercise [35] were not investigated, which is a limitation of the study. This study is significant in that it confirmed homogeneity by including all factors that affect sleep in the elderly, such as smoking, drinking, education, marital status, subjective economic status, and family members living together. The results of a study of osteoarthritis elderly living in a nursing home for sleep were effective in sleep supporting this study [23], pressure on five areas of shenmen, subcortex, sympathetic nerve, liver, and heart decreased PSQI by 2.26 points. Shenmen, sympathetic nerve (gyogam), and subcortex (pijilha) are pressure points commonly used to reduce sleep quality [18,23] and have been proven to be effective acupressure points for sleep quality. The quality of sleep is affected by musculoskeletal pain, and the more severe the pain and the longer the pain period, the lower the quality of sleep [11]. In Lee's study, elderly patients with osteoarthritis pain with a VAS score of 3 or higher were enrolled, and pain could not be controlled as a mediating effect on sleep quality [23].
Salivary cortisol levels were used as a physiological index to determine stress and psychological factors. In this study, morning salivary cortisol levels were measured, and cortisol levels decreased in the experimental group. AA therapy was applied to sinmun, gyogam, subcortex, and naebunbi for two weeks for middle-aged women to show stress, cortisol, and sleeping effects. In this study, cortisol levels decreased by 2.04 in the experimental group [19]. In addition, in this study, the effect of auricular acupuncture on depressed patients, shenmen, kidney, liver, lung, and sympathetic acupuncture for four weeks was found to be effective in reducing salivary cortisol levels and also effective in reducing suicidal ideation [9]. Depression in the elderly is a factor affecting suicide, and the effect of AA therapy on suicidal ideation should be verified in the future. AA therapy for three weeks lowered depression, anxiety, and stress in the elderly, improved sleep quality, and reduced salivary cortisol levels, which was also effective as a physiological indicator. AA therapy can be applied as a self management intervention for elderly individuals in the community due to its minimal pain and non-invasive approach.
Limitation
Since this study recruited subjects from a single institution and the sample size was small, it is necessary to reverify the results by expanding the number of subjects in a multicenter study. The physiological indicator cortisol exhibits a daily circadian secretion pattern that varies with time. To comprehensively assess it, multiple measurements are required across various times in the morning and afternoon. but there is a limitation in confirming the effect with a value measured once in the morning. This study separated the group visits in terms of time and space to maintain single-blind, but there is a limitation as it was conducted at one location in the senior center, and complete isolation was not achieved. In future research, it is recommended to utilize two or more facilities or vary the intervention timing to maintain single-blind.
CONCLUSION
The results showed that AA therapy was scientifically effective in relieving depression, anxiety, and stress in elderly individuals, improving sleep quality, and reducing salivary cortisol levels. This is significant because it has proven to be an intervention for the elderly in the community to maintain better psychological health. The justification for its use as a community nursing intervention is expected to expand.
Notes
CONFLICTS OF INTEREST
The authors declared no conflict of interest.
AUTHORSHIP
Study conception and design acquisition - Yoon H; Data collection - Yoon H; Analysis and interpretation of the data - Yoon H; Drafting and critical revision of the manuscript - Yoon H;
DATA AVAILABILITY
The datasets used and analyzed during the current study are available from the corresponding author.