Development of a Drainage Tube (Jackson-Pratt Drain or Hemovac) Management Protocol
Article information
Abstract
Purpose
This study aimed to develop a drainage tube management protocol for nursing students to enhance their core nursing skills and improve the quality of the nursing practicum.
Methods
A drainage tube (Jackson-Pratt drain or Hemovac) management protocol for nursing students was developed in four stages: a preliminary survey (stage 1), establishment of criteria for the implementation of the protocol (stage 2), finalization of the protocol (stage 3), and development of nursing scenarios to implement the developed protocol (stage 4).
Results
The final drainage tube management protocol outlined 23 steps, and the scoring system reflected whether each step was fully performed (2), partially performed (1), and not performed (0) for a total possible score of 46. The example nursing scenario was designed to evaluate the process through which nursing students provide care for a postoperative patient with a Jackson-Pratt drain (or Hemovac) with level 1 (fundamentals of nursing practice for sophomores in the first stage).
Conclusion
It is important to educate and evaluate nursing students on core nursing skills that must be learned and acquired during their school years, owing to their high frequency of use and importance in nursing practice. To this end, standardized protocols for each core nursing skill should be used to ensure consistent education and evaluation in nursing situations that resemble the clinical setting, in which continual updating of core nursing protocols is required.
INTRODUCTION
The Korean Accreditation Board of Nursing Education (KABNE) designated 20 core nursing skills with high frequency and importance to be essentially acquired during nursing education, and categorized these core basic nursing skills into advanced, intermediate, and beginner cate-gories for evaluation [1]. However, with the launch of the fourth evaluation phase in 2021, KABNE revised its approach. Instead of providing a protocol for the 18 core nursing skills, KABNE now presents only an overview of the difficulty level, objectives, prerequisite knowledge, and required supplies, and requires individual schools to implement a consistent and validated protocol for evalu-ating core nursing skills [2]. Drainage tube management, pressure injury management, fall prevention, and pain management have been modified or added, and protocols for these nursing skills need to be developed.
Drainage tubes are placed to remove secretions from body organs for various therapeutic purposes, and nurses perform several interventions involving drainage tubes, such as checking the positioning of the drainage tube, patency, and signs of infection. Previous studies [3-6] have reported that nursing skills education and training based on intentional protocols can enhance nurses’ nursing skills competencies. Therefore, drainage tube management education and training for nursing students is crucial for pro-moting the prevention and early detection of drainage tube-related complications. Additionally, valid protocols for managing commonly used drainage tubes, such as the Jackson-Pratt (JP) drain or Hemovac are essential for inclusion in the nursing practicum. Nevertheless, drainage tubes are managed according to the type of surgery, type of drainage tube, and guidelines at each institution [7]. Hence, a consistent protocol must be developed to ensure guideline-based, repetitive, and systematic education. Given this context, this study aimed to develop a drainage tube management protocol for nursing students to enhance their core nursing skills and improve the quality of the nursing practicum.
1. Literature Review
The historical evolution of drainage tubes can be traced back to the 5th century BC when an ancient Greek physician named Hippocrates recognized the importance of “ drain” in incising and draining abscesses [7]. Based on this, he attempted to perform a “ passive drainage” using gauze, metal, and glass tubes [7]. In subsequent centuries, there are records of various uses of drainage tubes, including the use of gravity drainage via metal intubation in the abdominal cavity by the Roman physician Celsus during the 1st century, and the discovery of the capillary effect in passive drains by Leonardo da Vinci during the Renaissance period [7]. Drainage tubes were further diversified in subsequent years with the introduction of the Penrose drain in 1890 and the development of the active drain by Heaton in 1889. Since 1947, suction drains have been used to prevent postoperative exudate pooling, and closed suction drains have been used since 1952 [7].
Wound drainage tubes have been used to prevent infection for a considerable amount of time, particularly in surgical patients. The absence of a drainage tube may cause certain wounds to appear externally healed while inter-nally harboring abscesses. However, empirical data have revealed that the incidence of site infections was 7.1% in patients without drainage tubes, 7.4% in patients with one tube, and 25.7% in those with two or more tubes, indicating a positive correlation between the number of tubes used and incidence of site infection [8]. Consequently, systematic management is imperative to optimize the bene-fits of drainage tubes while minimizing their adverse effects [9].
The fundamental concept of drainage tube management is consistent across the different types of drainage tubes, although some variations may exist. Nurses must ensure that the drainage tube functions properly and monitor for signs of infection or inflammation around the area [9]. Education on when to request drainage tube emptying, potential discomfort, situations where patients need to notify healthcare staff, and how to educate patients on the management of drainage tubes at home after discharge is essential [10]. The timing of drainage tube removal is controversial, but it is generally removed when the volume of drainage is less than 25∼30 mL per day or less than 1 mL per hour. Given that there is no standard duration for drainage tube placement, with varying criteria depending on the type of surgery, type of drainage tube, and the country and institution, the current practice is to adhere to the guidelines of each institution [7].
To reduce the risk of internal damage at the insertion site and minimize tissue irritation, drainage tubes should be made of a soft material that does not corrode or degrade. They should also be sufficiently sturdy to remain in place and be easy to remove. Drainage tubes are classified into two types: open passive drains (e.g., Penrose drains) and closed active drains, which are the most commonly used (e.g., JP drain or Hemovac). Closed active drains reduce the risk of microbial invasion through the tube into the wound and allow for accurate measurement of drainage volume [11]. These types of drainage tubes must be managed to maintain negative pressure in the reservoir to prevent it from expanding, and their patency must be maintained by squeezing each tube at an appropriate time to prevent blockage [7,8]. Furthermore, to prevent infection, hand hygiene should be maintained, gloves worn, and the drainage port should not be touched when managing drainage tubes, such as when emptying them [10]. Wearing personal protective equipment, such as an apron, can help prevent contamination of the drainage fluid and cross-contamination. Nurses are also instructed to continuously monitor and notify the provider in case of drainage tube dysfunction, sudden changes in drainage, or signs and symptoms of infection [11]. Therefore, basic drainage tube management skills for nurses in clinical settings should include understanding the roles and functions of different types of drainage tubes and anticipating and responding to changes in drainage and possible adverse events. In particular, the level of difficulty (medium) and objectives of drain management (explaining the purpose and process of drain management/gathering the supplies needed for drain management/performing drain management/docu-menting the results of drain management), a core nursing skill defined by the KABNE [1], must be considered when developing a drainage tube management (JP drain or Hemovac) protocol for nursing students.
Based on the literature review, the types of drainage tubes, management, and nursing interventions required for the development of a drainage tube management (JP drain or Hemovac) protocol for nursing students were discussed.
METHODS
The drainage tube management (JP drain or Hemovac) protocol for nursing students was developed in four stages-preliminary survey (stage 1), establishment of criteria for the implementation of the protocol (stage 2), finalization of the protocol (stage 3), and development of nursing scenarios to implement the developed protocol (stage 4). The drainage tube management protocol was developed between August 2022 and December 2022.
Stage 1. Preliminary Survey
In stage 1, the literature pertaining to evaluation tools for drainage tube management guidelines in Korea and abroad was searched. Relevant studies were collected from PubMed, Cochrane, CINAHL, and Web of Science. Additionally, the fundamentals of nursing textbooks were searched to confirm the specific procedures for drainage tube management.
Stage 2. Establishment of Criteria for the Protocol
In stage 2, the level of difficulty and objectives applicable to nursing students were identified. To this end, “ postoperative nursing” was referred to among the core basic purging skills described by the KABNE, which includes the skill of drainage tube management.
Stage 3. Protocol Development
The items in the protocol, supplies, and evaluation scoring were developed in stage 3. The content validity of the preliminary protocol items-that is, whether they reflect the latest knowledge and skills required in nursing practicum and education-was evaluated by three experts (one nursing professor with 20 years of teaching experience; one nursing professor with working experience as an infection management nurse; and one wound, ostomy, and con-tinence nurse). Each protocol item was rated on a four-point scale (1=not relevant at all, 2=not relevant, 3=relevant, 4=highly relevant), and the content validity index (CVI)-the percentage of experts rating the item as 3 or 4-was calculated for each item.
Stage 4. Nursing Situation Development
In Stage 4, nursing scenarios reflecting the actual clinical setting were developed to implement the protocol, and the relevance of the scenarios was evaluated by three experts (educational purpose, fundamentals of nursing practice for grade 2 in the first stage, nursing school lab en-vironment, and supplies).
RESULTS
Stage 1. Preliminary Survey
During the preliminary investigation in the first stage, we did not find domestic or international standardized practical guidelines related to drainage tube management, and there was no standardized protocol for nursing fundamentals in the nursing textbooks. Accordingly, it was confirmed that a preliminary protocol that is applicable to JP drain or Hemovac drainage tube management by utilizing the 4.1 edition of the core basic nursing skill evaluation protocol published by KABNE should be developed [12].
Stage 2. Establishment of Criteria for the Protocol
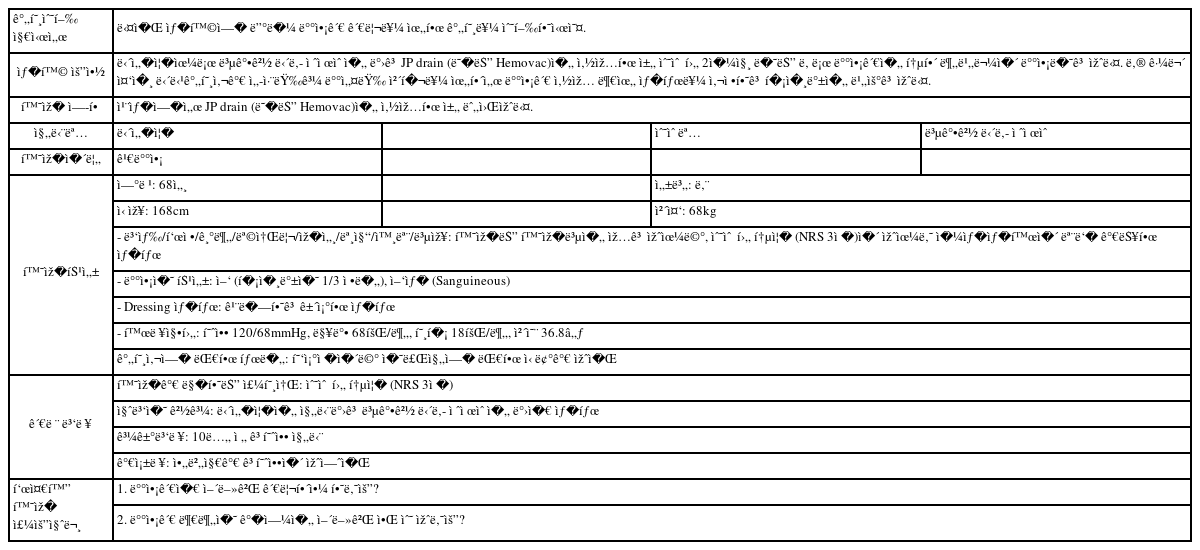
Following stage 1, the objectives and level of difficulty were set at “ medium” for drainage tube assessment and management based on the 4.1 edition of the KABNE core basic nursing skill evaluation protocol [12] (Appendix 1).
Stage 3. Protocol Development
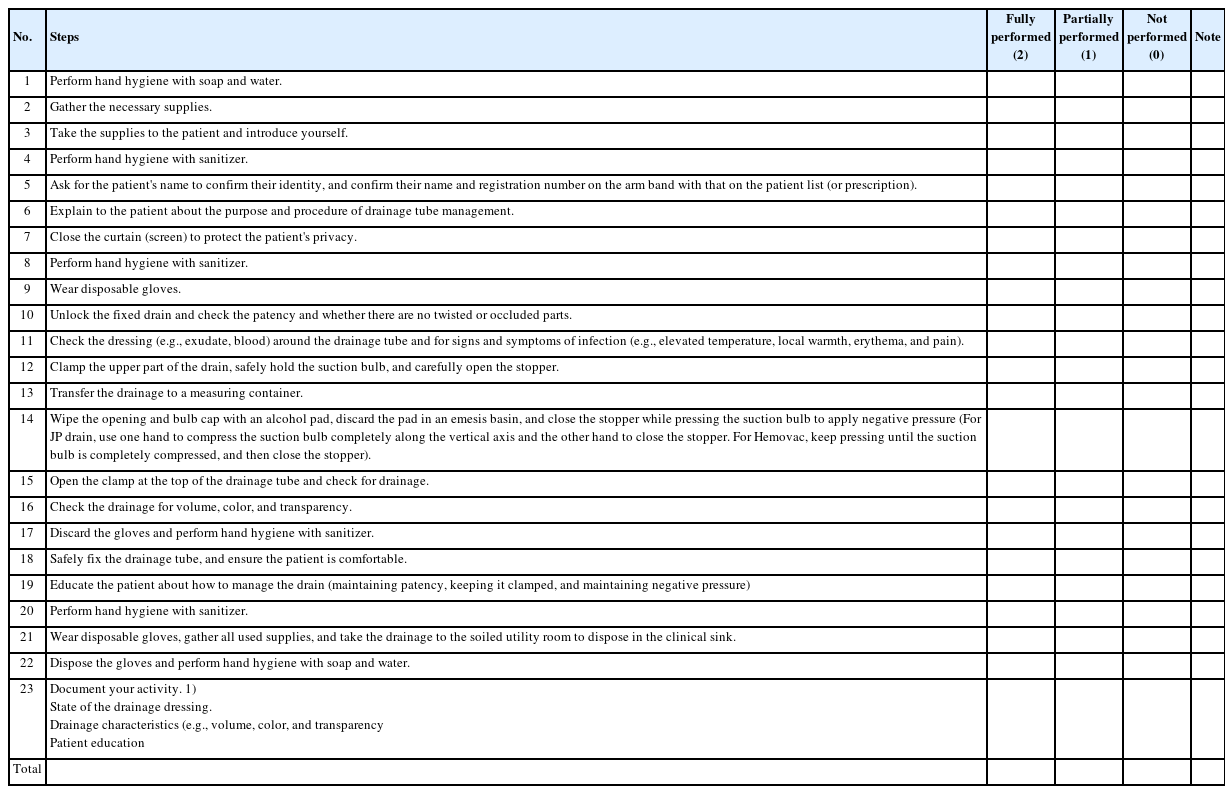
First, a preliminary protocol was developed by utilizing the 4.1 edition of the core basic nursing skill evaluation protocol published by KABNE [12]. The following procedures were added: 1) Number of times hand hygiene is practiced; 2) privacy protection of patients; 3) distinguishing between dressing conditions and infection symptoms and signs; 4) specific procedures for negative pressure formation by drainage tube type; and 5) patient education (maintaining patency, keeping it clamped, and maintaining negative pressure). The CVI of the preliminary protocol items was computed as 1, confirming good content validity [13]. In addition, the following items were revised by obtaining expert opinions: 1) Hand hygiene with water and soap separate from hand hygiene with sanitizer; and 2) redness as a symptom and sign of infection. The final drain tube management protocol outlined 23 steps, and the scoring system reflected whether it was fully performed (2), partially performed (1), or not performed (0), for a total possible score of 46 (Table 1, Appendix 2).
Stage 4. Nursing Situation Development
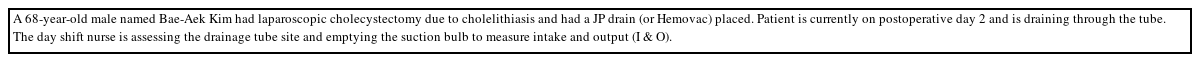
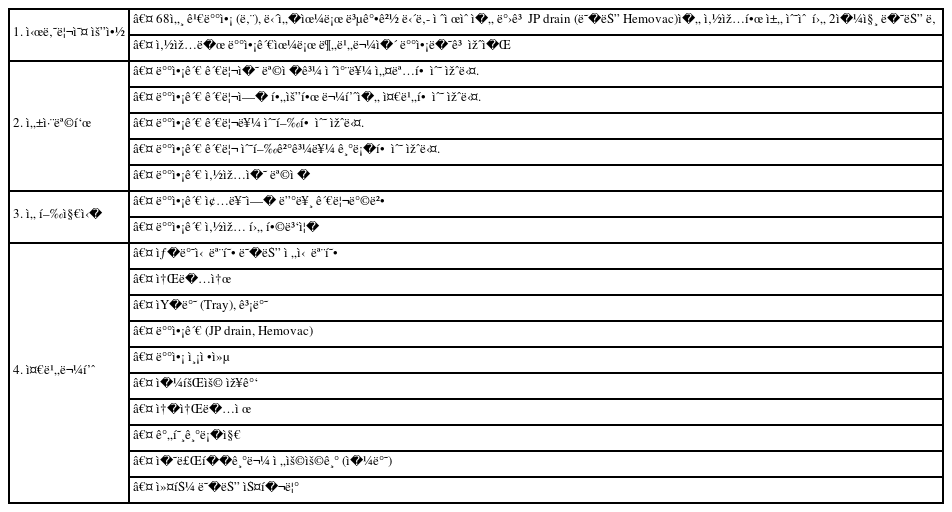
The example nursing scenario was designed to evaluate the process through which nursing students provide care for a postoperative patient with a JP drain (or Hemovac). According to the evaluation of three experts, the nursing scenario was found to be relevant in terms of the objectives, Level 1 (fundamentals of nursing practice for sophomores in the first stage), and nursing school lab en-vironment and supplies (Table 2, Appendix 3). In addition, the scenario was designed such that it could be modified and adapted to various real-world clinical situations.
DISCUSSION
This study aimed to develop a standardized drainage tube management protocol for nursing students to enhance their core nursing skills and improve the quality of the nursing practicum. To foster nursing students’ practical skills, the KABNE continuously evaluates core basic nursing skills based on the nursing education system [1]. In the 4th cycle (2021) of nursing education accreditation evaluation, “ drainage tube management” was proposed as a new core nursing skill based on a job analysis of new graduate nurses [2]. Thus, this study aimed to develop a validated protocol for drainage tube management to ensure a standardized and consistent nursing practicum, which is expected to contribute to repetitive and systematic nursing practicum.
In accordance with the objectives of “ drainage tube management” presented by the KABNE [1], the types of drainage tubes and scope of practice were limited to ensure Level 1 (fundamentals of nursing practice for grade 2 in the first stage). JP drain and Hemovac were chosen as the drainage tubes because they are the most commonly used in clinical practice [6,14] and require caution regarding negative pressures in the reservoir. The scope of drainage tube management was defined in terms of the frequency of practice and patient safety. Thus, the following items were adopted from the Core Basic Nursing Skill, 4.1 edition: checking the patency of the drainage tube, assessing the dressing for symptoms and signs of infection, emptying the drainage bag to measure drainage volume, and checking the drainage. The following items were added to address aspects that are often overlooked, such as hand hygiene, patient privacy, and patient education: item 7 (ensure patient privacy by closing the curtains [screen]), item 17 (taking gloves off and performing hand hygiene with a sanitizer), item 18 (fixing the drainage tube safely and ensuring patient comfort), and item 19 (educate patients on how to manage the drainage tube-maintain patency, close the cap, maintain negative pressure). We developed a Level-1 scenario involving a patient who under-went laparoscopic cystectomy and had a drainage tube placed, which was confirmed to be relevant by clinical experts. A protocol for drainage tube management (JP drain or Hemovac) was presented. The developed scenario and protocol were rated by experts as appropriate for Level-1 nursing students (fundamentals of nursing practice for sophomores), contained the latest knowledge and skills, and utilized specific action words such that the instructor could objectively assess students’ performance.
JP drain and Hemovac [7], the most commonly used drainage tubes, are circular, closed wound drainage systems made of silicone for suctioning exudates from surgical sites [15]. Maintaining negative pressure is essential for the proper functioning of the tubes. Without proper negative pressure, foreign substances can be introduced into the drainage site, causing infection. Therefore, nurses must manage the suction force by emptying the contents of the suction bulb and applying negative pressure on the wound suction bulb. Previous studies have provided use-ful evidence for maintaining negative pressure in a JP drain [16,17]. Therefore, we added specific instructions on how to compress the suction bulb vertically to the long axis of the JP drain in our protocol.
Generally, placing drainage tubes increases the risk of surgical site infections [7,18,19]. Preventing and managing site infections is crucial because they can lead to longer hospital stays, increased antibiotic use, and higher mortal-ity and morbidity rates [7,18]. Patients with drainage tubes have a six-fold higher risk of developing surgical site infections than those without drainage tubes [18], and fac-tors such as location, number, depth, and duration of drainage tube insertion have been reported to be significantly associated with an increased risk of infection [20,21]. However, many studies have found no statistically significant differences in infection rates between patients with and without drainage tubes [22-24]. In light of previous findings showing different patterns of microorgan-isms isolated from wounds, these conflicting results suggest that external contamination through drainage tubes is a possible cause of infection [25]. Therefore, nurses must adhere to standard precautions for drainage tube management and infection monitoring. Hand hygiene is the best way to prevent surgical site infections. Nurses should perform hand hygiene before and after touching the patient, before and after contact with drainage, and before and after wearing gloves, in addition to frequently changing gloves to prevent pathogen transfer to other parts of the body [26]. Nurses must also adhere to a series of infection management guidelines, such as avoiding touching the in-side of the suction bulb when opening or closing the drainage tube and cleaning the area with an alcohol swab after emptying the bag [27]. To assess surgical site infection, nurses should monitor whether the tube-site skin and dressing are clean and dry [28]; whether there are changes in the amount, color, transparency, and odor of drained fluid [26]; and whether they wear appropriate personal protective equipment (PPE), including gloves, to protect themselves from sudden exposure to body fluids [6]. The drainage tube management protocol, which includes these infection control principles, is expected to serve as specific learning material for nursing students to assess surgical site infections and prevent the transmission of infections related to drainage tubes.
Closed negative-pressure drainage tubes must be managed regularly to ensure that the suction bulb does not expand, and that the tubes are not blocked. Although this is the responsibility of the nurses who manage the drainage tube, the patient who has the tube placed should also check. In other countries, research and educational materials have been developed for patients with drainage tubes, including methods for emptying and measuring drainage, timing of drain emptying, maintaining patency (including removing impurities), identifying signs of infection, and seeking medical attention [9,29,30]. Educational videos on drain management and disinfection are also available in Korea for discharged patients; however, research on educational programs and materials for inpatients is scant. Therefore, we recommend that future studies develop and validate educational materials and programs for drainage tube management of inpatients.
This study has several limitations. First, we could not address open or closed drainage tubes other than the JP drain and Hemovac. Subsequent studies should develop standardized protocols tailored to different types of drainage tubes with varying roles and functions for use in clinical practice by nursing students. Second, the protocol lacks detailed nursing activities for identifying infections and inflammation around the drainage tube site and providing wound care. These activities are important for the prevention of complications due to drainage tubes and early detection of risks, but the “ drainage tube management” protocol developed in this study focuses mainly on emptying the drain. However, the basic scope of drainage tube management required by nurses in clinical practice varies across hospitals and attending physicians, making the consistent implementation of this protocol difficult. Nursing theories on drainage tube management suggest that nurses should check the wound while emptying the drainage tube [15]; therefore, further consideration is needed on how to practically implement this aspect of the protocol. Third, this study's protocol was designed for Level-1 nursing students (fundamentals of nursing practice for sophomores) and does not cover nursing actions for managing a blocked drainage tube, symptoms of infection and hemorrhage, maintenance of appropriate negative pressure, preparation for drainage tube removal, or methods of communicating changes in drainage volume and patterns within the healthcare team. Subsequent studies should develop nursing situations and protocols that pro-mote critical thinking in nursing students, including various issues in drainage tube management at varying levels of clinical nursing practices for third-and fourth-year nursing students.
CONCLUSION
It is important to educate and evaluate nursing students on core nursing skills that must be learned and acquired during their school years, owing to their high frequency and importance in nursing practice. To this end, standardized protocols for each core nursing skill should be used to ensure consistent education and evaluation in nursing situations that resemble the clinical setting, which requires continual updating of the core nursing protocols. In particular, despite the common postoperative use of closed suction drainage systems such as JP drains and Hemovac for surgical wound drainage, the drainage tube management guidelines vary across institutions, hindering nurses from providing quality care. Therefore, we aimed to address this issue by developing a standardized drainage tube management protocol.
Notes
CONFLICTS OF INTEREST
The authors declared no conflict of interest.
AUTHORSHIP
Study conception and design acquisition - Choi D, Lee H, Choi M-J, Kim K, Shin YH, & Kim J-S; Data collection - Choi D, Lee H, Choi M-J, & Kim J-S; Data analysis & Interpretation - Choi D, Lee H, Choi M-J, & Kim J-S; Drafting & Revision of the manuscript - Choi D, Lee H, Choi M-J, Kim K, Shin YH, & Kim J-S.
DATA AVAILABILITY
The data that support the findings of this study are available from the corresponding author upon reasonable request.