Effects of Obesity and Depression on the Incidence of Asthma in Korean Older Adults: A Secondary Analysis of the Korea National Health and Nutrition Examination Survey 2020
Article information
Abstract
Purpose
This study investigated the effects of body mass index (BMI), waist circumference (WC), and depression on asthma in older adults Koreans.
Methods
Data for 1,388 individuals (≥65 years) were extracted from the Korea National Health and Nutrition Examination Survey (KNHANES Ⅷ-2, 2020). Complex sampling design data were analyzed using stratification, clustering, and weights. Data were analyzed using unweighted frequencies, weighted percentages, estimated means and standard errors, the Rao-Scott x2 test, and multiple logistic regression analysis, which was performed to identify variables that influenced asthma after adjusting for confounding factors.
Results
The factors influencing asthma in the older adults were a depression diagnosis, age at the onset of depression, current depression status, and gender. In contrast, BMI and WC did not affect asthma. A diagnosis of depression had an odds ratio of 3.07 for asthma in the older adults. Furthermore, the odds ratios for asthma in the older adults were 5.08 for depression onset at <49 years and 3.37 for current depression compared to no depression diagnosis. The odds ratio for asthma in female older adults was 1.35.
Conclusion
The results of this study suggest that asthma in the older adults could be detected early through depression symptoms. This study also provides evidence that depression-related interventions should be included in asthma prevention and management programs for the older adults in Korea.
INTRODUCTION
Asthma is a chronic inflammatory lung disease, and the incidence of asthma in the older adults is increasing [1]. Asthma is aggravated by airway hyper responsiveness and changes in immune response due to aging [2-4]. The prevalence of asthma in the older adults is 7.8% worldwide [5] and 5.1% in Korea [6]. In particular, Korea has become an aging society, and the prevalence of asthma in the older population is expected to increase [1]. In the older adults, emergency room visits due to asthma are highest [4] and mortality rates are higher [2]. Asthma in the older adults is a very serious health problem. Therefore, it is necessary to prevent and manage asthma by identifying the factors affecting the incidence of asthma in the older adults [1]. Factors affecting the incidence of asthma include physical factors such as obesity [1,3,7-10] and psychological factors such as depression [11-14]. However, to the knowledge of this researcher, no study has investigated the effects of obesity and depression on the incidence of asthma in individuals aged ≥65 years in Korea.
Obesity-induced changes in immune function can cause inflammation in people with asthma and increase their susceptibility to viral infections [15]. Increased broncho-constriction symptoms in obese people are associated with decreased lung elasticity [16]. As indicators related to obesity, there are body mass index (BMI) (general obesity index) [9,16] and Waist circumference (WC) (abdominal obesity index) [8,10]. The BMI and WC were higher in the asthma group [3]. In particular, abdominal fat can better predict changes in lung function than BMI [8]. Abdominal subcutaneous fat was found to be associated with asthma [8,10]. However, obesity is not independently associated with asthma exacerbation in older adults, due to differences in the mechanisms that link obesity with asthma control in older vs younger adult [9]. In a study of older subjects in Korea, obesity was found to be associated with asthma in an unadjusted analysis, but obesity was not associated with asthma in the analysis after adjusting for sex, smoking, income, and other chronic diseases [17]. Previous studies [7-9,17] on the relationship between obesity and asthma in the older adults have shown various results. Asthma is riskier in the older adults than in adults [4,5]. Older patients with asthma have higher airway neutro-penia, but these characteristics are not commonly observed in adult patients [9,10], and central obesity and loss of skeletal muscle mass are characteristics of aging-induced geriatric obesity [3]. Accordingly, the risk of asthma due to obesity may be altered by factors such as aging [4,5]. Although asthma and obesity in the older adults are increasing, few studies have confirmed the relationship between obesity and asthma in the older adults [1,8]. Confirming this relationship can provide additional insights into the relationship between these factors in the Korean older population.
Depression is associated with asthma, and depression is higher in older patients than in adults with asthma [12,13]. Depression is a major mental health problem, and 13.5% of people aged 65 or older in Korea had depressive symptoms. In particular, by age, 75∼79 years old (15.6%), 80∼84 years old (19.7%), and 85 years old or older (24.0%) were found [18]. In the older adults, depression reduces lung function and increases airway inflammation [12]. Additionally, depression not only increases the incidence of asthma [14] but also affects dysregulation in patients with asthma [19]. Older patients with depression and asthma have lower scores on asthma control tests [11]. Depression can worsen asthma by reducing awareness and adherence to asthma treatment [19]. As depression leads to poor asthma control [11], asthma-related hospitalizations have increased in older subjects [1]. On the other hand, asthma improved when depression was relieved [20]. Therefore, it is necessary to identify and provide depression intervention for e older patients with asthma.
In a previous study of asthma in the older adults, obesity, and abdominal obesity (AO) were found to be related to asthma [7,8]. On the other hand, studies in Korea [17] and the United States [9] showed that obesity did not affect asthma. In addition, most of the asthma studies [9,16] did not differentiate between adults and the older adults. However, obesity's impact on asthma prevalence may be agedependent [9]. In a study of asthma and depression in the older adults, Korean subjects [22], and in foreign subjects, African Americans [12], Germans [13], and Chinese [20], there was an association between depression and asthma. Depression-related factors may confound the association between obesity and asthma [9]. Asthma morbidity is high in the older adults [2], who are diagnosed late, making control difficult [1], but research is relatively scarce [2]. Therefore, it is necessary to study the effects of obesity (physical factor) and depression (psychological factor) on the incidence of asthma in the older adults. This study aimed to provide evidence for asthma prevention and early treatment by identifying the effects of obesity and depression on the incidence of asthma in the older adults in Korea.
METHODS
1. Research Design
This descriptive research study analyzes the National Health and Nutrition Examination Survey to investigate the effects of obesity and depression on asthma in the older adults in Korea.
2. Participants and Data Collection
The participants of this study were the older adults (≥65 years), and their data were extracted from the eighth National Health and Nutrition Examination Survey data (KNHANES VIII-2, 2020). A two-step cluster sampling method was used to extract data of the participants in the KNHANES VIII-2. In the first stage, sample surveys were selected, and in the second stage, households were selected. The cities/provinces, dongs/eup-myeon, and housing types were stratified based on the extraction frame, and the residential area ratio and householder's educational background ratio were used as implicit stratification criteria. The KNHANES VIII-2 data consisted of health questionnaires, physical examinations, and nutritional surveys, and trained staff collected data from 7,359 participants. In this study, according to the raw data open and care regulation of Korea Centers for Disease Control and Prevention, after the researcher got confirmation for using data (February 10, 2021), the data was provided, and the study period was from June 2021 to December 2022.
This study analyzed the data of the final 1,338 out of 7,359 participants, excluding non-responders (252) and those under the age of 65 years old (5,769). Asthma diagnosis group was 130 participants (weighted 9.1%), and non-asthma group was 1,208 participants (weighted, 90.9%).
3. Measures
1) Asthma definition and disease-related characteristics
Asthma was defined as characterized by respiratory symptoms such as wheezing, dyspnea, chest tightness, and cough with variable expiratory airflow limitation [1]. Disease-related characteristics included asthma diagnosis (“ Have you ever been diagnosed with asthma by a doctor?”), asthma onset age (<50, 50∼59,≥60), current state of asthma (yes, no), asthma treatment (yes, no), asthma drug administration (regular drug administration, irregular drug administration, no drug administration), smoking status (non-smoker, ex-smoker, current smoker), amount of smoking (cigarettes/day)(1∼10,≥11) and starting age for smoking (≤20, 21∼35,≥36)
2) Obesity
In KNHANES VIII-2, to measure the participants’ total body obesity, height and weight were measured after fasting overnight and wearing light clothes. BMI is the weight divided by height squared (m²) [23]. According to the classification criteria for obesity of the Centers for Disease Control and Prevention [23], in this study, normal weight (BMI <23 kg/m²), overweight (BMI=23∼24.9 kg/m²), obesity (BMI=25∼29.9 kg/m²), and severe obesity (BMI ≥30 kg/m²) were classified. WC measurements were taken midway between the last rib and the iliac ridge, which was not the maximum WC in KNHANES VIII-2 [23]. The cut-off point for WC for defining AO was ≥90cm for male and ≥85 cm for female [24].
3) Depression
Depression-related characteristics included depression diagnosis (“ Have you ever been diagnosed with depression by a doctor?”), depression onset age (<50, 50∼59, ≥60), current state of depression (no, yes), and depression treatment (treatment, no treatment).
4. Ethical Consideration
This study was conducted with the approval of the Hannam University Institutional Review Board (IRB no. 2021- E-03-02) for the secondary analysis of the KNHANES VIII-2. The KNHANES VIII-2 data collection was conducted by experienced experts through health questionnaires and physical examinations. The data applied top-coding, bot-tom-coding, and re-categorization methods to ensure anonymity and confidentiality of personal information.
5. Data Analysis
This study analyzed by creating an analysis plan file with stratification, clustering, and weights applied. The participants’ general characteristics indicated unweighted frequencies, weighted percentage, estimated mean, and standard error. Differences in general characteristics, BMI, WC, and depression between the asthma diagnosis and non-asthma groups were analyzed using the Rao-Scott x2 test. Multiple logistic regression analysis was performed to identify the variables that influenced asthma after adjusting for age, gender, education level, smoking status, amount, and starting age. WC was converted to a binary variable differently for each gender (male; WC ≥90 cm=1, WC <90 cm=0; female; WC ≥85 cm=1, WC <85 cm=0). Since the WC converted into a binary variable can apply different AO criteria according to sex, the reliability of multiple regression analysis can be increased. The adjusted odds ratio and 95% confidence interval for each variable were calculated (SPSS 26.0, IBM Corp., Armonk, NY, USA).
RESULTS
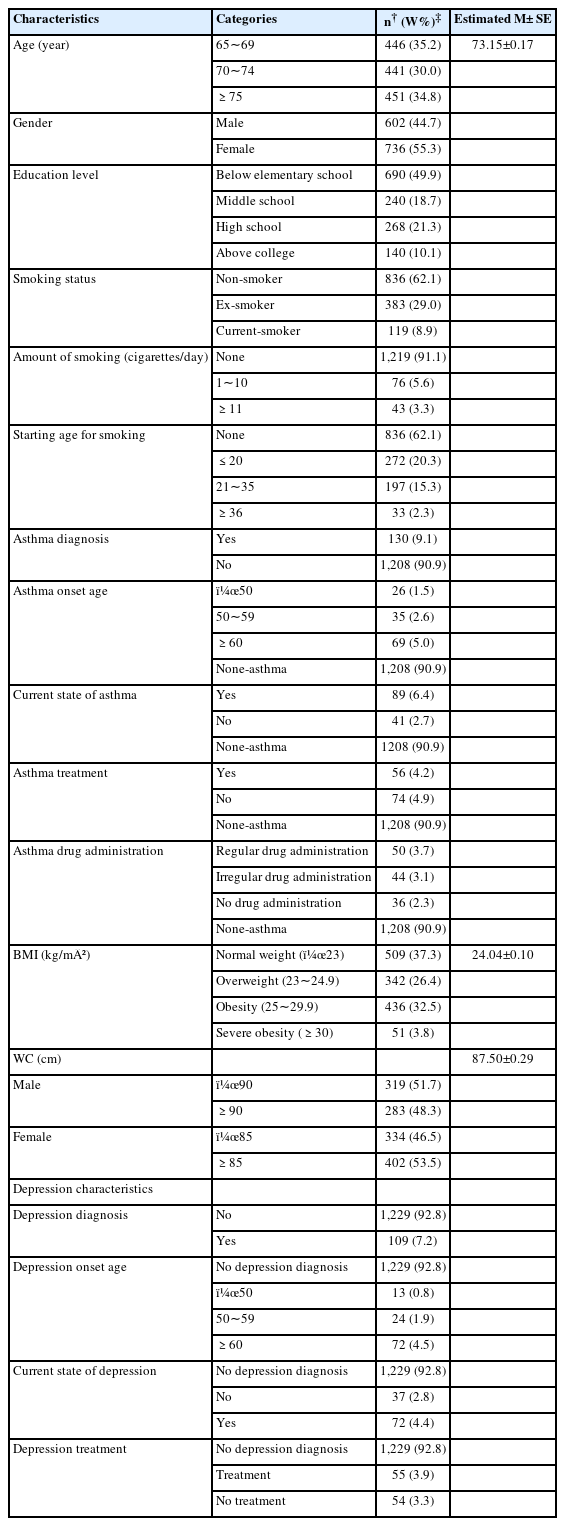
1. General Characteristics of Participants
The mean age of participants was 73.15 years. Male (n = 602, 44.7%) and female (n=736, 55.3%) were representing. Educational level less than elementary school represented the highest proportion (n=690, 49.9%). In total there were 836 (62.1%), non-smokers, 383 (29.0%) ex-smokers, and 119 (8.9%) current smokers. Among current smokers, 1∼10 cigarettes were the most common. In the age of starting smoking, it was most common ≤20 years of age.
The asthma diagnosis group comprised 130 (9.1%), and the age of onset of the participants was the most common at ≥60 years of age (5.0%). Current asthma was found in 89 (6.4%) of participants, and 74 (4.9%) of cases were not treated, while 56 (4.2%) were treated. For asthma medication, the order was regular, irregular, and no medication.
The participants’ mean BMI was 24.04 kg/m² and WC was 87.50 cm. The diagnosis rate of depression was 109(7.2%). Among this group, the depression onset age was most often ≥60 years. Current depression was found in 72(4.4%) (Table 1).
2. General Characteristics of the Asthma-diagnosis and Non-asthma Groups
In the asthma diagnosis group, 82 (62.1%) of female and 48 (37.9%) of male which was a significant difference from 654 (54.8%) of female and 554 (45.2%) of male in the non-asthma group (x2=5.12, p=.028).
Age, education level, smoking status, daily smoking amount, and smoking onset age were not significantly different between the asthma diagnosis and non-asthma groups (Table 2).
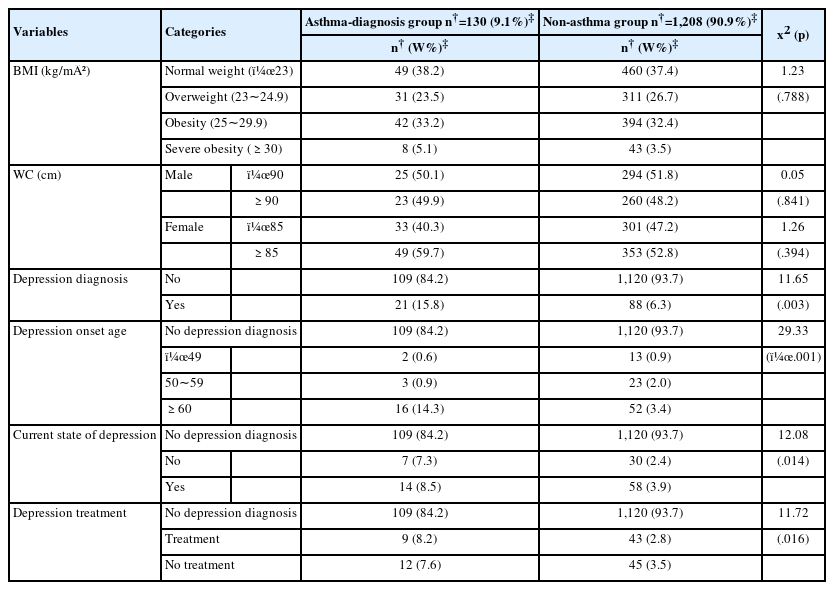
3. BMI, WC, and Depression-related Characteristics of the Asthma-diagnosis and Non-asthma Groups
There were no significant differences in BMI (x2=1.23, p=.788), and WC (male, x2=.05, p=.841; female, x2=1.26, p=.394) between the asthma diagnosis and non-asthma groups.
Depression was diagnosed more frequently in the asthma group than in the non-asthma group (x2=11.65, p=.003). The age of onset of depression ≥60 years was higher in the asthma diagnosis group than in the non-asthma group (x2=29.33, p<.001). Current depression (x2=12.08, p=.014) and no treatment for depression (x2=11.72, p=.016) were higher in the asthma diagnosis than in the non-asthma group (Table 3).
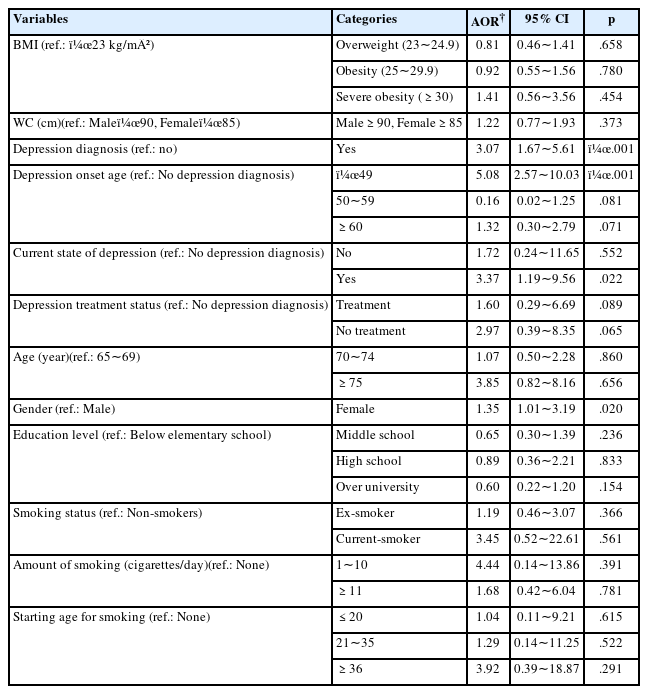
4. Factors Affecting Asthma in Older Adults Koreans
The factors influencing asthma in the older adults were depression diagnosis group, age at depression onset, current depression status, and gender. The odds ratio for asthma was 3.07 times (95% CI=1.67 to 5.61, p<.001) for depression diagnosis group, 5.08 times (95% CI=2.57 to 10.03, p<.001) for depression onset at <49 years, and 3.37 times (95% CI=1.19 to 9.56, p=.022) for current depression compared to no depression diagnosis.
The odds ratio for asthma was 1.35 times (95% CI=1.01 to 3.19, p=.020) for female. In contrast, BMI and WC were not factors influencing asthma in the older adults (Table 4).
DISCUSSION
This study investigated the effects of physical (BMI, WC) and psychological (depression) factors on asthma in older individuals in Korea and determined that the factors influencing asthma were depression diagnosis, age at depression onset, current depression status, and gender.
In this study, depression diagnosis was more than three times higher in the asthma group. In a study on African Americans [12] and Germans [13], those with asthma had a higher risk of depression than non-asthmatic participants. In a study of older adults, chronic respiratory diseases such as asthma were associated with a 1.53-fold increase in depressive symptoms [25]. In a Korean study, depression diagnosis was associated with a higher asthma prevalence [22], and in an American study, depression was a marker for the risk of incident asthma [14]. In a Chinese study, asthma risk increased by 4% for each 1-point increase in the Center for Epidemiologic Studies-Depression score [20].
Asthma and depression share pathophysiological mechanisms mediated by genetic susceptibility and immune-inflammatory pathways [25]. In addition, mechanisms by which depression may induce asthma include central and autonomic nervous systems’ actions, and depression is associated with autonomic dysregulation in the form of cholinergic activation, leading to airway constriction [20]. This hypothesis [25-27] can explain the mechanism by which depression causes or increases asthma. Previous research [12,13,20,22] and this study showed that depression affects asthma. Therefore, evaluation of depression is necessary for early asthma detection in the older adults. In addition, interventions for depression should be included in asthma management for the older adults.
In this study, BMI and WC were not significantly different between the asthma diagnosis and non-asthma groups and were not factors influencing asthma in the older adults. Obesity was not related to asthma after adjusting for gender, smoking, income, and depression [9,17]. There was a significant relationship between BMI and asthma only in those aged <65 years [15,21]. Our study adjusted for age, gender, education, smoking, and depression-related variables and similar results were obtained. In this study, depression-related factors were associated with asthma, and these factors may confound the association between obesity and asthma. On the other hand, asthma was higher in obese older adults [7] and was associated with airway hyper responsiveness [16]. Central fat was associated with asthma risk regardless of BMI [10]. Previous studies on the older adults [7,8] did not adjust for factors such as depression. Therefore, it was thought that the results were different from those of this study. Also, in a study of young adults, obesity increased both the prevalence and incidence of asthma [15]. The risk of asthma increased 1.4 times for BMI (30.0∼34.9 kg/m²) and 2.5 times for BMI (≥50kg/m²) [21]. This is because there are pathophysiological differences between asthma in young adults and the older adults [9]. Our findings differ from those of studies on asthma and obesity in young adults [15,21]. Further studies are needed to confirm the difference in obesity-asthma dynamics between these age groups. Identifying the mechanisms by which obesity affects asthma in the older adults will help improve asthma treatment and develop targeted interventions specifically for older adults [9].
In this study, asthma was 1.35 times higher in female than in male. The prevalence of asthma is higher in males before the age of 14 years and higher in females with advancing age, and the cause of the difference in asthma prevalence by gender is unclear [1]. This is because depression causes more asthma exacerbations in female than in male [28]. In addition, obesity is more associated with asthma in female [21], and abdominal and general obesity are associated with asthma in female but not in male [29]. In other words, female with depression, which are asthma-related factors, had a high incidence of asthma.
This study showed a stronger association between asthma and depression in the older adults than previous studies [12,13,20] because we adjusted for confounding factors using multiple logistic regression. As a limitation of this study, since the diagnosis of asthma is self-reported, accurate diagnosis of asthma can be difficult due to omission, and the causal relationship between obesity, depression, and asthma cannot be identified through a cross-sectional study. BMI and WC are indicators for evaluating obesity, but these two variables have a high correlation, and also, depression-related variables and smoking-related variables can have multicollinearity. In future studies, it is necessary to supplement multicollinearity by performing univariate and multivariate analyzes on obesity-related variables (BMI and WC), depression-related variables, and smoking-related variables, respectively. In addition, in the study of the effect on the incidence of asthma in the older adults, studies excluding cases of onset before the older adults are needed.
Asthma symptoms in the older adults are regarded as normal aging and diagnosed late [1]; in this study, it was confirmed that depression management was important for the older adults with chronic diseases such as asthma. It also provides evidence that interventions related to depression should be included in asthma prevention and management programs for the older adults.
CONCLUSION
In conclusion, this study is clinically useful in that it provides empirical evidence that depression diagnosis and management should be included in intervention programs for the prevention and management of asthma in the older adults in Korea. In addition, asthma is a danger-ous disease that obstructs the respiratory airway, and it is educationally useful by presenting evidence for the necessity of nursing education on asthma symptoms, preventive methods, and influencing factors for early detection of asthma, especially in the older adults.
In this study, the effects of asthma on the older adults were investigated after adjusting for confounding factors. However, the analysis of obesity and depression together is a limitation since one can act as a confounding factor for the other. Therefore, to confirm the effect of asthma on the older adults, it is necessary to confirm the unadjusted and adjusted results. We suggest further studies to confirm the differences in the epidemiology of obesity, depression, and asthma in adults and the older adults.
Notes
CONFLICTS OF INTEREST
The author declared no conflict of interest.
AUTHORSHIP
Lee H contributed to the conception and design of this study, performed the statistical interpretation, drafted the manuscript and critically revised the manuscript. All authors read and approved the final manuscript.
DATA AVAILABILITY
Dataset files are available at https://knhanes.kdca.go.kr/knhanes/sub03/sub03_02_05.do